Are Your Cues Holding Your Clients Back?
Introduction
One of the most common questions I get asked when teaching my courses is “what cue do you use to teach this?” It’s an interesting question to answer because the answer is always “it depends on the client in front of me”. Think back to the exercises and how you learned them - do you use some of the cues that you were taught? Certainly the answer will be “yes” for all of us in some way as well as using new ones we either made up or acquired along the way.
Jane’s Story
Let me tell you a little about Jane (name changed for privacy) - Jane’s story is a common one I have heard from patients, clients, physios and fitness professionals from around the world...maybe you have a “Jane” as a client? Jane has 2 primary school-aged children and is a healthcare professional working in the hospital system. She has moved a few times for husband’s work, juggling running the family and working full time. She had good post-natal physiotherapy for some stress-urinary incontinence, diastasis and participated in physio-led exercise classes with good results. She currently has thoracic and lumbar back pain, urinary urgency and pelvic pain during intercourse (dyspareunia), particularly in prone lying - which is also an aggravating position for her back pain. She was seeing a MSK physio for the back pain, a Women’s Health Physio for her urgency and dyspareunia, and a Pilates Instructor for some Pilates-based exercise. She asked for a consult with me to take a broad approach to her problems because she had 3 different exercise programs, 3 different sets of cues for her “weak core and pelvic floor”, and she still couldn’t lie prone, enjoy sex nor exercise or pick up the children because of the different pains and urgency. She had 2 physios and a fitness professional that weren’t talking to each other and didn’t understand what the others were asking her to achieve...a tricky situation!
A Problem Of Cueing Or A Problem Of Our Underlying Beliefs And Model?
Have you ever wondered if what we were taught is actually helping our clients? I was trained to focus on activating and coordinating muscles and joint movements. My cueing was “internally focused” (more on that later!)...it was what I was taught to do and seemed to produce results (look up post hoc ergo propter hoc fallacy for more information on why results aren’t proof of why something works or why someone gets better!). Much of what I was taught to do both in my undergraduate degree and in my post graduate Masters in Manual Therapy were based on the Postural / Structural / Biomechanical Model (PSB). The current evidence-based practice model is a BioPsychoSocial Model (BPS). Our words, language and cueing all stem from our beliefs and training.The words we choose can indicate to us if we are working in the older PSB model or in a more BPS model. Lederman (2010) “The Fall of the Postural / Structural / Biomechnical Model” and “The Myth of Core Stability” are good review articles and ones that were influential in changing my approach.
The Hierarchy of Competence
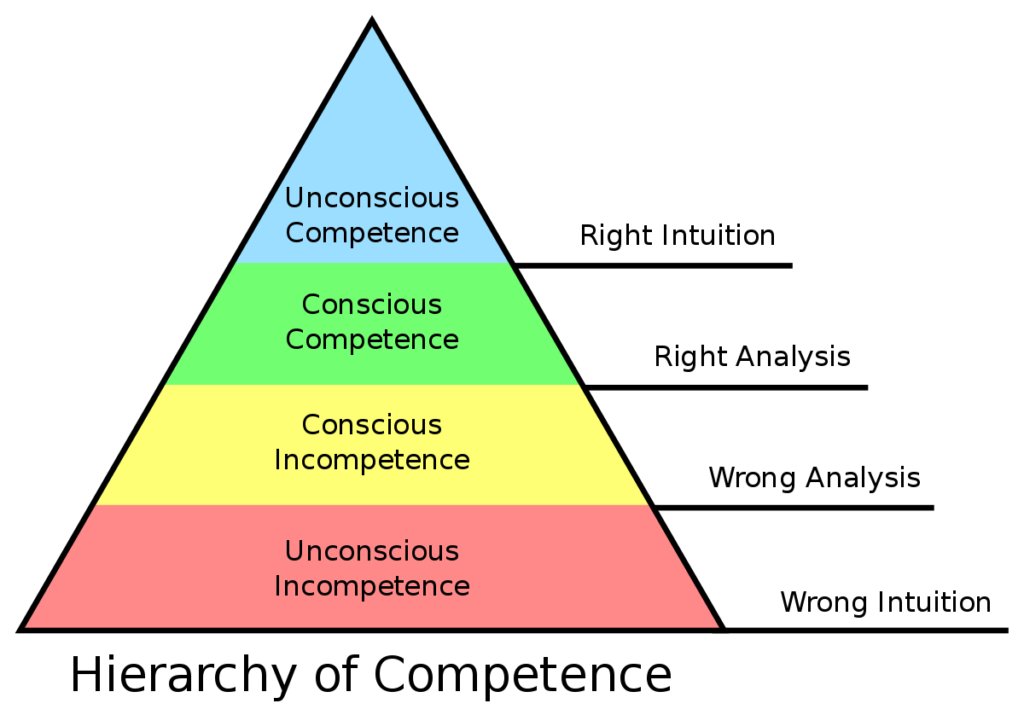
We clinicians tend to use internal cues from a well-intentioned desire to help our clients but the reality is that we often leave our clients at “conscious competence” - this is often seen as always cueing someone to activate a muscle like their “core”, “pelvic floor”, “glutes”, or whatever body part you draw attention to. Broadwell (1969) and later Burch (1970s) developed The Four Stages of Learning, also known as the Hierarchy of Competence:
- Unconscious Incompetence - the client doesn’t know what they aren’t doing “correctly” - they’ve never had to think about using their “core”, “pelvic floor”, “glutes” before and now someone is telling them that they aren’t using them properly and it is the source of their woes! Aren’t we are good at drawing attention to these things in our clients?!
- Conscious Incompetence - now the client is aware that they are doing things “incorrectly”, they now are focused on every time they do anything and are left wondering “I’m probably not doing it ‘right’ because I am sore”. Never mind the fact that it probably isn’t that relevant to their condition, they now know they are doing something “wrong”.
- Conscious Competence - We work hard with them to teach them how to “activate correctly” or use the “right technique” - often using fancy and expensive toys like real-time ultrasound (RTUS). They are now able to do what we want (yay!) and we ask them to always think of their cue before executing the activity or exercise or action. This is where we physiotherapists are really good at getting people to and leaving them here.
- Unconscious Competence - to truly help someone achieve their goals, we should try to get rid of the cues as soon as possible. “Normal Function” is just thinking about what you want to do and doing it, not actually stopping to think about a cue first...and yes, there are some who may need to think about it but cues are behaviours and behaviours can be trained to become as automatic as possible.
Types of Cueing
Cueing affects attentional focus and have been described in 3 varieties - internal, external and natural. An internal focus and cue is one that focuses on body parts and movements e.g. “use your core”, “ activate your glutes”, “don’t hold your breath” . An external focus and cue is one that focuses on the outcome or movement effect e.g. “stand up”, “keep the barbell moving vertically”. A natural focus is likely to be an internal or external focus and is often based on the client’s beliefs and training from healthcare and/ore fitness professionals. “Focus” is what you direct your attention to (internal, external or natural). “Cues” are the directions given to direct your focus and attention.
What Does The Research Say?
The research actually indicates that external cues produce better results for skill retention - which is what we physios would like to see our clients do, to truly change their behaviour to achieve the goals they want. Novices tend to do better with “external focus” than “natural focus” but experienced clients do better with “natural focus” compared to “internal” or “external focus”. The area of attentional focus, cueing and performance vs learning is a very interesting one. Winkelman (2018) “Attentional Focus and Cueing for Speed Development” is an interesting read and a good start for delving deeper into the research regarding attentional focus and cueing.
A Radical Idea
What if we could simply summarise what we do as physiotherapists as simply “Do Something Different”? We do our subjective and objective assessments, decide what deviates from our “expected norms” and give the client a different experience by changing what they usually do. We help change their movement patterns, thoughts and beliefs, perception with our manual therapy and “toys” (electrotherapy, RTUS etc). Why not focus on what the client is strong at, what they are capable of doing, what they are adaptable to, and how resilient they are? What if we focused on using those strengths to achieve their goals instead of pointing out all the “wrong” things they do which may not actually have any relevance to their presentation?
External focus and cues should be tried first, not just one or two times but spend the time using analogies and different variations. I prefer my clients experience change before I do “patient education” - once they have that experience, the education/information part has a more meaningful context. However, I also acknowledge that sometimes an internal focus or cue is needed...if so, please try body part movements (eg. change in body position), not muscle activations. Watching someone trying to contract “the right muscles” during an exercise or movement produces rigid, unathletic movement and results! Once your client is getting the basic technique you are looking for, then progress within minutes, not weeks, towards unconscious competence.
Back To Jane’s Story
After listening to Jane and her story, I discovered the following:
- She had a lot of beliefs both from her healthcare training and from the providers she consulted. This had led her to fear certain movements and positions as well as be prescribed many exercises and cues, which she assumed should allow her to progress towards her goals and what she wanted to do.
- She was “bearing down” during her pelvic floor contractions - this is unhelpful as it puts added pressure onto the pelvic organs and may contribute to her feelings of urgency, especially during activities and exercises.
- She lay prone with lots of muscular activity and some pain. She could lie prone with pillows under her hips with less muscle activity and without pain.
- She was able to move, squat, and pick up weights without fear or pain if she used different techniques.
My intervention and cueing for her was as follows:
- I talked to her about her goals and we worked together to plan her progression back to what she wanted to do.
- With the pelvic floor cue, I used analogies like “imagine a sleeping baby holding your finger” to get the responses (less activity) I wanted and tested them as best I could using external palpation medial (but not midline) to the pubic ramii, ischial tuberosities and sacrotuberous ligament. (Since I was only monitoring for bearing down, this sufficed but an internal examination would be ideally be needed to confirm this)
- I showed her that she can lie prone with pillows without pain and it was an option for intercourse. By the end of the session, she was able to lie prone without pillows and without pain. The cue was simply to “relax and let the pillows support you”.
- Since she was fearful, we started with some internal focus and cues during movement, squatting and picking up weights - “how does it feel while you lift and move?”, “keep your chest over the weight”, and “Use as little tension you can to get the job done” (because she believed she had to contract things strongly). As she began to experience that it doesn’t have to be painful, we moved immediately into external focus cues like “stand the weight up”.
She had 2 sessions with me where we talked a lot and ceased a lot of the exercises and cueing she had. She no longer has dyspareunia or urge, she is able to lie prone to sleep and for intercourse without pain and her back pain is only occasional, mild and easily modifiable. Most importantly, she has less fear, better beliefs about her back pain and pelvic floor dysfunctions, and has a better understanding of cueing from those beliefs.
Conclusions
- Our cueing comes from our beliefs and model we use to interact with the client.
- We often tie down our clients with unhelpful beliefs and don’t progress them to unconscious competence.
- External focus and cues are better than internal ones for all abilities.
- Internal cues may be needed to start a client off if external cues aren’t getting the job done.

Thx Antony. Love your style and learn so much from you. i will read again and again and share.
Hi Kathy – thanks for the comment and for sharing – I hope it helps. Let me know future topics you want me to write about. Cheers
I am alarmed and (ashamed of my profession) that Jane was seeing a “women’s health” Physio who hadn’t done an internal and re-educated her on her incorrect PF technique!
Thanks Donna. To be fair, I had a word count so couldn’t put absolutely everything in there. She did have an internal and was told she did them correctly but I suspect that “Jane” just overdid it and lapsed into her usual habit of bearing down.
The bearing down was quite obvious for me from the external examination so I didn’t have to fret about if I was making up the palpation findings or not.
I think the thing that helped “Jane” the most was the broader view I took and ensuring she understood each finding and how it related to her conditions in a holistic way. It simplified things for her and only gave her a couple of things to think about instead of lots of things from 3 different perspectives which were a bit confusing because they were different from each other without obvious reasons why it needed to be different.
Cheers for the comment.