SIJ Series – 1.What is the SIJ?
Hi - this is the first of a series of short blog posts to get you acquainted with your SIJs. Let me know what you think...
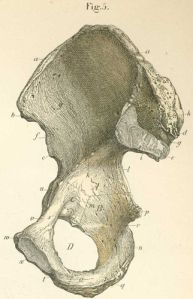
There are many Myths and legends about the SIJ. Some people believe that all problems come from the pelvis (which are the 2 SIJs, the pubic symphysis and the innominates (2x Ilium, Ischium and Pubis).
The Sacroiliac Joints (SIJ) are 2 of the most important joints in the body. They transfer the load from the lower limbs (your legs) to the spinal column. If they don't do their job properly, you will start to load unevenly through your body.
Uneven loading in the body can lead to hip and knee joint arthritis, disc injuries in the back and pain from strained ligaments around the SIJ.
Research suggests that the SIJ is the *cause* of pain in 15-20% of low back cases...but just because the SIJ is sore doesn't mean it is the main problem...
Do you have what might be SIJ pain? Why don't you leave a comment and tell us about your story.
If you are a physiotherapist, why don't you go to www.myPTeducation.com to find out where the next SIJ is being held - if you want us to come to your town/city to run one, just email Antony at antonylo@mypteducation.com or leave your comments below.

SIJs should definitely be looked at as part of any program for back pain. We have a particular interest in this given its also the initial/primary site of disease for many patients with inflammatory spinal pain, axial spondyloarthritis (labelled Ankylosing Spondylitis in later stage radiological disease). Do you see a lot of spondyloarthritis given your interest in SIJ?
Hi Irwin – or should I call you Dr Lim?? 🙂
You ask good questions.
Firstly, I don’t see a lot of spondyloarthritis or AS. I judge this based on the fact that most of my patients don’t present with persistent unresolved inflammation and the common symptoms of AS. If they have joints that feel stiff (rather than compressed), then I start to get a bit worried but the number of these patients is very low in the 11 years+ I have been in private practice.
I use a diagnostic paradigm that focuses on function and efficient load transfer. I am always looking for what the different regions are doing from an Articular (joints, ligaments, bones, cartilage, etc), Myofascial (muscle bulk, contractile elements, fascia, etc) and from a Neural (CNS, PNS, motor planning and coordination, etc) point of view. It is also focused on functional activities and incorporates a biopsychosocial approach to ensure we assess and treat the patient as holistically as possible.
In my opinion, often the SIJ is painful and in fact is the pain producing structure (PPS) but I look more for the cause for the PPS.
The SIJ becomes the main or Primary Driver of the problem when I can demonstrate through my testing and assessment that the SIJ is the first region to fail load transfer – that is to do something not biomechanically efficient which leads to other joints/regions failing load transfer.
I then look further into the Primary Driver to determine the reason/s why it is failing – as described above.
AS should (and has) shown up through this process. I have been fortunate to have most of these patients present with a diagnosis already. I have only found it in one patient on my own – presented as back pain but quite stiff, in his 20s, no good reason for the pain. XR of spine showed features of AS so I sent him back to the GP and he was sent to a Rheumatologist.
How does your group deal with SIJ problems?
Just call me Irwin. Do keep an open mind about spondyloarthritis. Many patients take close to a decade from onset to be diagnosed and I think the figures suggest that most have seen a number of physios along the way without diagnosis.
The symptoms are often intermittent at least in the early years. Xray changes can take a decade to manifest.
So, the key would be inflammatory features & in particular, worry if:
a) buttock pain, either side or alternating at different episodes
b) night pain, particularly if waking up in 2nd half of the night
c) early morning stiffness, improvement with activity
d) associated features: psoriasis (rash or nails), peripheral joint disease, enthesopathy, recurrent tendinopathy, inflammatory bowel disease
Most of these patients, particularly young males (late teens onwards) are often told its mechanical & there’s usually something to blame eg sport or lifting, given these events do still trigger the underlying problem.
Sorry to go on about it but it’s hard to not mention this when your blog is going to be about the SIJ. I’m suprised you’ve only diagnosed 1 in 11+ years given you see so much of SIJ dysfunction.
The prevalence is estimated to be 1/200 to 1/1000 with 5% of chronic back pain sufferers having thought to have spondyloarthritis.
So, it’s common.
Thanks Irwin – Fantastic information. Please feel free to add more!
As a Rheumatologist, I am certain you would know more about it that I.
I would be the first to be happy to admit that perhaps I don’t catch all the spondyloarthritis (SA) patients but I do have patients who go on to see a Rheumatologist and have blood tests etc.
The 1 in 11 years was an AS patient. I am sorry i switched from SA to AS in the previous comment.
Your work with the recent World AS Day has highlighted and reminded me about Spondyloarthritis so i really appreciate your input here.
Apart from medications, I would think that my management would be similar to what I have been doing thus far – assessing their functional activities, identifying the dysfunctions, classifying and working out the path to normal function and implementing it using appropriate techniques and activities. Would that be right?
For the readers out there, Arthritis Australia put out information sheets. This link has the one for Spondyloarthritis – http://www.arthritisaustralia.com.au/images/stories/documents/info_sheets/english/colour/Spondyloarthritis.pdf
I am happy for you to put your details here Irwin – I haven’t done so since I didn’t have your permission 🙂
Your assessments & therapy don’t have to change. Just consider the diagnosis & earlier referral to your rheumatologist of choice as the assessments & medical therapy have changed a lot.
Feel free to contact me to discuss any cases. BJC Health has developed a lot of specific expertise in spondyloarthritis/ankylosing spondylitis.
Hope the Singapore course goes well.
Good site! I really love how it is easy on my eyes it is. I am wondering how I could be notified whenever a new post has been made. I have subscribed to your RSS feed which may do the trick? Have a nice day!
hi burn fat quick – you can subscribe via email which will let you know as well 🙂 thanks for the support 🙂 Cheers!
I have had SI pain along with back pain for many years. No good dx. I am beginning to suspect that I may have undiagnosed AS as I started having intense SI aching at night long before when I was a teenager in the mid-seventies. I found that putting my mattress on the floor helped and just lived with it. However, when I went to a chiropractor in 1995 for neck pain and headaches, that aching got almost unbearable for a while as he stirred things up. Then one day, after he adjusted my SIJ’s (probably because I was complaining), something shifted in my pelvis within 24 hours and back muscles came on. I have had a bigger, more constant problem since.
What would it do for me to go to a rheumtologist and see about the AS? I am already doing everything I can to maintain a strong core and upright posture. The aching comes from time to time, but I think that my main problem is something else…..perhaps secondary to presenting with undiagnosed AS to a chiropractor. Now I am very careful. Even Reiki can upset the apple cart!
You are a bit far away for me to come consult with you. I am in the US. Are you familiar with the work of Richard DonTigny?
Thank you! Interesting site!
Hi Wendy,
Thanks for the comment – I would definitely check out some medical diagnoses first – something isn’t right if even Reiki can upset things. If all of those things prove to be negative (a proper, thorough check of your medical systems), then certainly consider musculoskeletal physical therapy.
Perhaps you could email info(at)discoverphysio.ca to see if they have a physical therapist that they have trained in your city/town. Obviously replace the “(at)” with “@”.
I haven’t heard of Richard but I will look him up.
Stay in touch – glad you enjoy the site.
Cheers