SERIOUS WARNING – If you do any releases to your Psoas or Abs, you MUST READ THIS
 Today, I want to tell you a story of something that happened to a good friend of mine this weekend...but first, some context...
Today, I want to tell you a story of something that happened to a good friend of mine this weekend...but first, some context...
Does this sound familiar?
You roll up to the gym, you grab a roller or ball and start rolling out. After your gym/CrossFit/whatever session, you might be back onto the roller or ball again with some stretches as well.
With the massive increase in "mobility" exercises, drills, and not to mention "things" you can buy to help release muscles, more people than ever are interested in keeping their body in good shape and releasing muscles - This is a good thing.
I have been around the world and there is a disturbing trend - coaches, those who aren't qualified health professionals, are helping people release by stepping on them (presumably to avoid any accusation of "massaging") or just helping them "release" their muscles including Psoas.
This is a DANGEROUS thing!
It is up to you whether you want to do this as a coach - is it covered by your insurance? If you are a client, again, it is up to you - what happens if things go wrong? Ideally, you should get a health professional to help you release your muscles, especially in the abdomen... The other joints - I understand. money is an issue, it seems all the same (it isn't), you can't be bothered, etc. I am truly ok with people trying to take care of themselves.
What I want you to do is just understand the risks...and then I will treat you like an adult that can make their own decisions.
 Karin's Story
Karin's Story
Karin (not her real name) is an old friend of mine. She has had some issues in the past that I have helped with. Karin trains at the local globo gym and has seen other health professionals as well. I personally haven't treated or seen Karin for ages...literally 8 months ago.
Karin told me she saw someone last week twice and during that time there were lots of "adjustments" and her "Psoas" was released fairly aggressively (Karin's description). This therapist has a good reputation and is well trained and it could have easily been me, a physio, a chiro, a massage therapist or osteopath (except I don't go aggressively for Psoas...more on that later). The point is that Karin became unwell after seeing a well qualified therapist...she didn't just ask a friend to help her...she did the right thing and the therapist did as well.
Anyway, Karin felt unwell after the session and got worse, such that she threw up twice within half an hour. She tried to put up with it (she is a tough girl) but couldn't get any sleep that night and every time she moved, she had severe pain. She still had the vomiting and now diarrhea. When she contacted me, I told her to go straight to emergency as I thought she had a ruptured appendix.
Basically, she did.
When they operated on her, she they took it out and found it had a small rupture in it.
Now, it could be that it was ready to go and a sneeze could have set it off but she had this pain since straight after the treatment and it only got worse. That is part of the risk of working in the abdomen - whether it is Psoas or Iliacus or whatever deep structure you are going for. There is a lot going on in there.
The following is to help outline some of the reasons - anatomical and philosophical - why I don't get stuck in like I used to (and was taught to). This is not about someone rupturing an appendix - I think that it might have contributed to the situation but probably wasn't the only reason.
Why I Don't Aggressively Release the Psoas
1. RARELY is the Psoas the primary problem or the primary contributing factor. I often find that the psoas is reacting to something and I would rather treat that "something" and then on the retest, the psoas is happier and MUCH LESS pain for the patient
 2. You can't effectively get to it in most people without causing lots of pain. When I go looking for it, I start by trying to find the anterior spine (you can feel your spine through your tummy!). A guy my size, forget it! I will hit you before you can get deep enough to feel my spine. Most people have a Psoas that is roughly in line with the front of their spine, maybe a little bit of it anteriorly...but to get any sort of pressure on the muscle, you are going to have to get to at least below the line of the anterior body of the vertebra...not happening in a lot of people...maybe a skinny girl. I have done it before but the pain is significant and causes the patient to tense up so the effect is almost worthless.
2. You can't effectively get to it in most people without causing lots of pain. When I go looking for it, I start by trying to find the anterior spine (you can feel your spine through your tummy!). A guy my size, forget it! I will hit you before you can get deep enough to feel my spine. Most people have a Psoas that is roughly in line with the front of their spine, maybe a little bit of it anteriorly...but to get any sort of pressure on the muscle, you are going to have to get to at least below the line of the anterior body of the vertebra...not happening in a lot of people...maybe a skinny girl. I have done it before but the pain is significant and causes the patient to tense up so the effect is almost worthless.
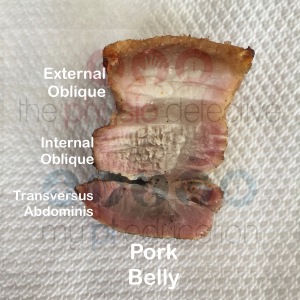 3. I suspect a lot of people need tender spots in their rectus abdominis and obliques worked on. If you are a high level athlete, these muscles can be quite dense - have a look at pork belly. We have a similar abdominal wall. You have to get through all those abdominal muscles and then the internal organs before you get to psoas. Like point 2 above, it is not easy to get to.
3. I suspect a lot of people need tender spots in their rectus abdominis and obliques worked on. If you are a high level athlete, these muscles can be quite dense - have a look at pork belly. We have a similar abdominal wall. You have to get through all those abdominal muscles and then the internal organs before you get to psoas. Like point 2 above, it is not easy to get to.
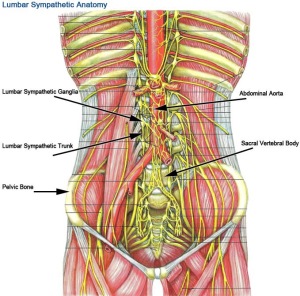 4. The Sympathetic Trunk lies right next to the Psoas. If you manage to get to the Psoas, you might irritate these important nerves. These nerves control your internal organs from your heart, lungs, skin, bowels, sexual reproduction organs, etc. Irritating them can make you feel ill, nauseous or sick.
4. The Sympathetic Trunk lies right next to the Psoas. If you manage to get to the Psoas, you might irritate these important nerves. These nerves control your internal organs from your heart, lungs, skin, bowels, sexual reproduction organs, etc. Irritating them can make you feel ill, nauseous or sick.
 5. The Genitofemoral and Femoral nerves along with the gray rami communicates (small spinal nerves) are also around and through the Psoas muscle...this can cause shooting pains and altered sensations like pins and needles.
5. The Genitofemoral and Femoral nerves along with the gray rami communicates (small spinal nerves) are also around and through the Psoas muscle...this can cause shooting pains and altered sensations like pins and needles.
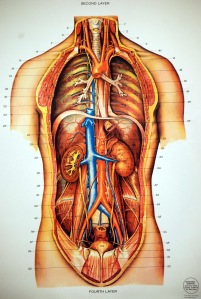 6. The Abdominal Aorta and Inferior Vena Cava are major blood vessels that run along the spine. These are usually resilient but some people have an abdominal aneurysm. If you poke around looking for the psoas, you can kill someone by rupturing it. The Abdominal Aorta then branches into the Common Iliac Arteries. These arteries lie in front of and next to the Psoas muscles...if you feel a pulse, DON'T RELEASE IT!
6. The Abdominal Aorta and Inferior Vena Cava are major blood vessels that run along the spine. These are usually resilient but some people have an abdominal aneurysm. If you poke around looking for the psoas, you can kill someone by rupturing it. The Abdominal Aorta then branches into the Common Iliac Arteries. These arteries lie in front of and next to the Psoas muscles...if you feel a pulse, DON'T RELEASE IT!
 7. The intestines are all over the Psoas. They usually just get out of the way but sometimes they can get pinned down. To experienced hands, intenstines feel like hollow sausages and definitely feel different to the psoas muscle. But it is a subtle distinction. In Karin's case, she probably had a low grade, "grumbling" appendix that got irritated and ruptured from the release. Have a look at the picture. You have to get through the muscles of the abdominal wall and then all of this viscera and then past the blood vessels before you get to the psoas.
7. The intestines are all over the Psoas. They usually just get out of the way but sometimes they can get pinned down. To experienced hands, intenstines feel like hollow sausages and definitely feel different to the psoas muscle. But it is a subtle distinction. In Karin's case, she probably had a low grade, "grumbling" appendix that got irritated and ruptured from the release. Have a look at the picture. You have to get through the muscles of the abdominal wall and then all of this viscera and then past the blood vessels before you get to the psoas.
 8. Ovaries, uterus and kidneys are also in the area. You can rupture an ovarian cyst, irritate endometriosis scars, or bruise kidneys, the ureters or bladder. Look at the photo - you have to get through A LOT to get to Psoas.
8. Ovaries, uterus and kidneys are also in the area. You can rupture an ovarian cyst, irritate endometriosis scars, or bruise kidneys, the ureters or bladder. Look at the photo - you have to get through A LOT to get to Psoas.
So What Should You Do?
1. Use an experienced degree-trained health professional who has experience in knowing about the internal organs and muscles. To be honest, Osteopaths traditionally are taught "visceral manipulation". Some physios and chiros (like myself) have done courses on how to "listen" and take care of viscera. These courses are often restricted to physios, chiros and osteos...that is not to say your massage therapist isn't trained, it is just much more unlikely. Hopefully the above list gives you an idea of what I am thinking about when I examine that area. The unfortunate situation is that even experienced therapists doing the right thing might aggravate things. I don't think Karin's therapist was negligent but from what Karin has told me, the pain got worse after the treatment. Like I said earlier, it could have been ready to go and anything could have set it off.
 2. Use a broad-based object like a kettlebell handle, roller or ball to release your abdominals - forget about trying to get the psoas. Honestly, you have to solve why they are getting jacked up, not just try to beat them into submission.
2. Use a broad-based object like a kettlebell handle, roller or ball to release your abdominals - forget about trying to get the psoas. Honestly, you have to solve why they are getting jacked up, not just try to beat them into submission.
3. The pain should be tolerable, like a 2-3/10. There are usually better things to go hunt down than pounding your abdominal wall. If I do decide to proceed with a painful treatment, it is for a good reason and I explain it and demonstrate using test-retest why it was done. Even if it is for 30secs, I am wary of painful treatments.
4. Proceed with caution. Don't just let anyone stick their fingers or foot or implement into your guts. If you feel sick, throw up or have diarrhea after treatment, get thee to the hospital ASAP!
Karin's Story and Conclusion
Karin is recovering in hospital still as I write. She had to stay in a few days with IV antibiotics because the appendix ruptured and leaked into her abdomen. She will make a full recovery and eventually be able to train again but recovering after abdominal surgery means that her training is interrupted for at least 6 weeks. [update - she developed an abscess and now has to have a drain inserted and an extra 5 days in hospital]
We love doing things that "hurt so good"...damaging internal organs shouldn't be one of them!
Please take care in the future of what you choose to release and why. There are many ways to "release" your psoas... It takes a comprehensive assessment to work out why it wants to lock up. Find someone who knows what they are doing...if you can't find someone, you can always contact me.
You are an adult - take this information and make an informed decision. Discuss it with your coach and health care team. Make sure that if you are truly interested in taking care of your body, that whatever you do to it and whomever you let "release" your Psoas, knows what they are doing and have taken the above information into account. Even then, as with Karin's story, treatment can still flare things up.
I would be interested to hear your thoughts on what I have presented above - have you honestly thought about these issues before? Will Karin's story change your views on what you do to your Psoas?

Great post A! I hope it will be part of your book:)
Marianne Ryan PT, OCS MRPT Physical Therapy http://www.mrptny.com Phone: 212-661-2933
>
It seems as if those who believe that they “release the psoas” are unable to see the many contraindications for poking around in the abdomen, trying to get to the psoas muscles. Someone can die on your table if you poke through their abdominal aorta or vena cava or their bifurcations. You can damage a client’s kidneys or ovaries, or their genitofemeral nerve or other arteries, veins, nerves, etc., that lie over the iliopsoas muscle. You can puncture the colon, which does not move, and which stands between you and your vulnerable client’s psoas. Why does this bounce off so many hard heads? You are massaging the recIt is indeed a strange phenomenon. And it is no insignificant problem for competent massage practitioners. Both of the schools I attended recklessly taught students to “release the psoas.” One school showed a brief video of the abdominal viscera but still encouraged the misinformed practice. The truth is, rampant incompetence plagues the practice of therapeutic massage. How can it ever recover? The best we can do, I guess, is continue to do what you’ve done here, and point out the need for competent education and evidence-informed practice. One (that I know of) of my clients came to me injured from “psoas massage” and was thankful to find someone thoughtful and knowledgeable enough to avoid causing her any more harm. Thank you for your post of sound information, the more of which gets out to practitioners, the better.
Thanks Jen.
I do think the viscera and arteries are pretty hardy in most people but there are risks in some populations.
They are not as hardy as you might think. I listened to a surgeon describe her handling of them, and, according to her, they should never be blindly poked around in at all, to try to mash the psoas, or for any other reason, by anyone who doesn’t understand that.
Yep but we have a whole abdominal wall and skin and fat between us and the intestines 😉
Anthony what is the best way to contact you? Wanted to discuss further options with you and brain storm.
Use the contact us option on the page is best. Cheers
In the middle of that first post, I was trying to say, you are massaging the rectus abdominus and obliques and perhaps the colon, usually, and not the psoas muscle, which is too posterior to reach from the anterior abdomen.
If you approach the psoas from an appropriate angle, you will avoid the Rectus Abdominus. The author makes a great point though that there are many other obstacles and dangers. This is why manually massaging the psoas is my last option, and I prefer to use the 4 other techniques I have.
Have you tried the options of not trying to address the psoas? They work too 🙂
Wow, I was scared before now I’m really scared. I was injured at work a year ago, was in alot of pain never heard such load cracks and pops from my back or anyone’s for that matter. Went to the chiropractor the day I was injured, could barely walk, if I stood stationary I would have to take my left hand place it at the back of my thigh to move my leg. After a few treatments I was getting better, relapsed once in the years time up until roughly four weeks ago. Started getting a slight pain in my hip, then down my leg, severe muscle cramps in thigh and calf of leg. I’ve notice if I keep moving it’s not too bad. Sleeping is almost impossible, the pain never subsides. Yesterday morning I awoke and the inside of my knee hurt, yesterday I was completely miserable, kept getting light headed and my mo events were extremely slow…. Today I woke up not much better, my knees was hurting more, felt like it was jammed and I noticed it was swollen. My movement is getting much slower, I look like I just had surgery when I walk, hope that makes sense, the light headedness is coming more often and I started feeling sick to my stomach, feeling of throwing up kept arising. Went to my appointment with the chiropractor, he was out today, and he had another doctor there to cover. He checked me over, worked on my mine left leg , did the release by pressing down on my stomach explained things very well and told me to get and MRI cause I have lost motion in my hip. He said I’m to young to have hip problems, get the imagine as soon as possible. I’m glad he was there today, I found out alot. I have been researching this issue all day. I’m feeling so sick, but I know it wasn’t from him I felt this wayong before I went to my appt. What.advice do u have for me.. Thank you for telling Karen’s story, very helpful.
Sincerely,
S. Bailey
Anthony, I never usually comment online, but what u wrote re psoas is so important. I wouldn’t let anyone work on me there, anyway. Since I read recently abt the psoas, been doing CRP every evening. Fortunately, there is no pain. U see, I’m looking for a safe, maybe 3 good core exercises to do. Maybe u can help me with my burning question : is yoga sun salutation, &, is the ( elbow) plank, r those 2 okay for the psoas ? Or not. Maybe even good for it, or no. The internet doesn’t know. Maybe u do:-) I’m already working on my posture. I greatly appreciate ur article, & ur site. If u can, thx for answers to question. If not, I understand. Best wishes & Gratitude
Thanks for the information. Yesterday, I made a decision to visit a physical therapist for some pain that I acquired through years of heavy lifting. She did all kinds of strength tests in which I believe only 1 caused me discomfort. I was told to lay on my stomach as she pressed on each side of my lower lumbar to free up L1 and L2 which were supposed to be blocked. It felt phenomenal as she was hitting the spot, but when I went to roll on my back I got a cramp right were she was pressing. I could not walk!! I had to struggle for an hr just to try to get to my feet. I finally found enough strength to slowly walk to warm that area up. I still don’t know what it is but was a very scary experience. I thought I was going to have to call an ambulance to take me out of there.
That sucks david. It sounds like she irritated a nerve by accident – lots in the area! Hope you are feeling better now. Thanks for sharing!
Hi Anthony
Thanks for your informative and well researched article. I am a massage therapist with 24 years experience with training in Neuromuscular therapy. I would agree completely that the iliopsoas needs a great deal of care and attention while working the area, especially considering all the delicate nerve and venous tissue that is around it. However, I would like to add that I have found that working the Iliopsoas directly very valuable, especially with people who have chronic LBP. I often find trigger points in the muscles and once these are cleared the LBP generally will improve. Like any technique working the area takes practice and it took me years to feel comfortable with it. Now I’m able to go in quickly and gently and with lots of presence of mind, confidently. Thanks again. Charles McGrosky CMT (USA) ps Enjoyed your podcast on the physioedge.
I agree with you Charles. I too am an RMT, and treating the psoas happens to be a specialty of mine. The article outlines basically why most massage therapists won’t touch the area. It’s too bad, becuz most people do need treatment. We have become a society in chronic flexion, and the root seems to be in the hip girdle.
I hope this article doesn’t scare people away from receiving treatment, or make therapists reluctant to do the treatments.
Hi joyce and charles.
Sure, it does help some people but have you ever had a client feel worse after your massage? It isnt because they needed to get worse to get better. One very common reason is that you released the lrotective muscle spasm which was protecting them from going into hip extension or posterior pelvic tilt or lumbar flexion.
Let’s look at it a different way.
They come in and you decide that thomas test is positive. You want to “release” the psoas because it is “tight”. One of 3 things can happen:
a. It gets better. Can you really add true length to a muscle in an hour? If the muscle is truly shortened and it’s length is a problem causing pain by limiting movement, i would suggest that massage won’t make the muscle longer and the reason why they felt better is because you affected the muscle activity via neurophysiological pathways…which means other methods can also work instead of direct pressure. They can also get better because your massage might have affected an organ or nerve or anything else I listed (or didn’t mention) because there is no truly direct way ti the psoas. At the best, you have to go through the muscles of the abdominal wall – what if you really affected their external oblique which stopped pulling on the ribs which stopped irritating the iliohypogastric nerve via the sinuvertebral nerves which run up to 4 levels above and below vertebral level, which can affect the rami communicans which can affect transversus abdominis which can affect spinal stability which can cause protective muscle spasm of the psoas? That’s just one possibility. I sincerely doubt you lengthened the muscle otherwise massage would fix people with contractures.
b. It gets worse. I would suggest you may have damaged something (possible but not likely in healthy tissue) or you release protective muscle spasm which allowed the client to move into a position of aggravation.
c. It stays the same. Despite your best efforts, the psoas wants to stay in that level of activation which means that whatever it is protecting is more important than the stretching, massaging and whatever you did during the session. If you see this, refer straight away to a physio for further assessment because belting away at the muscle won’t solve the problem.
I am not saying that massage isnt effective. I am saying that it isnt always the answer and sometines when it does help, it isnt for the reasons why we think…and that goes for physio and chiro and osteo techniques too.
What do you think – happy to discuss it more.
Sounds like you really know your stuff Anthony!
Most often I find there are trigger points in the psoas and iliacus, and when these points are released, the pain decreases (and often disappears), and the client is then able to stretch it. I have encountered tight psoas muscles where when applying some pressure to it will allow the muscle to relax…and it literally melts under my fingertips. Sometimes, it is a trigger point in the obliques, in which case, I address them. I’ve never really thought that treating the psoas would lengthen the muscle, per se, but more of a releasing it from an extreme contracted state. The lengthening happens with stretching…so I will often stretch that while they are on the table, and give them instructions on how to do it at home.
So whether I am releasing the muscle from a contracted state or affecting neural activity, I don’t know. Most people want relief NOW, so I do what I need to do! I have psoas issues myself, and I only find relief with direct pressure on it. I tend to have lumbar pain when the psoas is in spasm, as do most of my clients. Stretching it is just about impossible, becuz it just hurts!
In regards to how I treat the psoas and iliacus….some would call it aggressive, becuz I’m digging in there, but it’s done with great care. The approach is slow and communication with the client is imperative. I make sure I don’t push on the colon or intestines (they move out of the way if you go slow) and certainly avoid organs. I start at the bottom of the psoas and work my way up. I have the client positioned with their legs bent at the knee to take tension off the abdominal area. To ensure I’m on psoas, I have them slowly lift their leg a bit. Iliacus is easier to access with less chance of pushing on anything we shouldn’t be…..and I often find that just by getting the triggers on iliacus is enough to remove the pain.
The only other ways I’ve had mine treated is with muscle energy and contract-relax. Neither worked for me, and I’ve tried the contract-relax with clients with no change.
But if you look at the bigger picture, a tight iliopsoas often presents with tight glutes, hams or quads…and sometimes all the above. Addressing them all, as well as giving appropriate exercises to the client is necessary. I’ve instructed my clients to adjust their seats in their cars, or work to encourage better posture.
I’m open to suggestion on other ways to ‘release’ the psoas!
Trigger points? Tender spots, yes.
Why would it want to be in an “extreme contracted state?” What would be the purpose?
Is the Psoas truly short? Or just overactive?
How would you release a muscle from a contracted state if it is not affecting neural activity?
I have no doubt you are effective…I just want people to question why what they do works. Quite often, the reasons are not what we think.
As for your Psoas, why do you think it resists so much to your self treatment and stretching? You say your back is sore when your Psoas is in “spasm” but what if your Psoas is in spasm because your back is sore? Are you treating the right thing?
As for the bigger picture, I am all for that.
“Releasing” Psoas is not would I would aim for. I aim to make change to people’s systems – I often think about how to enter their brains via the classical articular system, myofascial system, neural system, visceral system, psychosocial and strategies for technique and function. This model is the integrated systems model and can be found in Diane lee’s book the pelvic girdle.
I suggest you find the primary contributing factors that are causing the issues you are observing 🙂
Cheers
There are two positional releases for the psoas, one of which involves holding the leg in a position which shortens the muscle and waiting until the client relaxes and “lets go” of the tension or effort to help you hold it there. The other involves moving the leg into a position which puts a gentle stretch on the psoas and waiting for gravity and the client’s abdominal breaths to slowly release the contraction and lengthen. The latter of these two is obviously more efficient (when it works) because you can go work on something else while the psoas is releasing. You can find a demonstration of this technique here: https://youtu.be/GD0UNaEVwD4
You can also use Proprioceptive Neuromuscular Facilitation (PNF) to release the psoas, or use a therapist assisted passive stretch or an active stretch.
Or you can just get moving and do something different 🙂
What I meant to include in that last post was this: No one technique works every time for every client. Different bodies react/respond differently to various stimuli/techniques. Therefore it is useful to have a as many tools in your toolbox as you can. Given what Anthony has pointed out about the risks involved in direct manual manipulation of the psoas, perhaps the other 5 techniques should be tried first.
Or maybe just don’t bother treating the psoas. I don’t remember the last time I needed to…exercise is stronger than any manual therapy…
I also am a internationally Board Certified Neuromiscular therapist. I attended a sports science school in undergrad then went to premed then chiropractic school then went to in to the only school other than the one in Europe who focuses on NMT. Sadly it had been sold and the couple who are both highly respected Doctors and researchers retired and sold the school now is it a massage school where you get a dash of NMT. I agree there are many therapist out there who have no business touch or working many parts of the body as they lack the knowledge and those who get a dusting of NMT should not be allowed to call themselves neuromuscular therapies because they are not. They have not had the training and this upsets me To do so and can cause more harm than good. However with that said if you know your A&P you can treat the psoas and illiposoas effectively without harming your client. I have been working on the psoas for over 15yrs and have physical therapist, orthopedics and chiropractors refer people to me that they can not help and get results. But the key is knowing orgin and insertion and what other muscles are “tied” to them and you need to know the persons health history. What type of work they do hobbies sleeping position past injuries even it they were 30ura ago because old injuries especially major once can rear their heads years down the road But if you are trained well and know the body inside and out you should not have any problems treating your client.
Hi Pamela. I believe you can work on the psoas. The bigger question is “why”?
What exactly are we hoping to achieve?
To answer those questions, we need to examine the philosophy we base our beliefs in.
Just because you have had success treating in whatever paradigm you have used doesn’t validate the reasoning why it worked.
All paradigms, including the ones I teach, are just stories to try explain the clinical phenomena we have observed. I’m very honest about what we know to be “true” and the truth is that most paradigms don’t hold water.
“But I get results! Isn’t that the most important thing?” – maybe. At what cost?
I can go on and on.
All this to say “examine why you believe working on the psoas is necessary”. I haven’t worked directly on psoas for a long time. Still getting results (quickly too I might add) and it came about by challenging myself to prove myself wrong.
If I can help people get better by doing basically the opposite of what my paradigm tells me to do, what does that mean about my paradigm?
Anthony,
Your point about paradigms, models, philosophies, and stories is a good one and I agree that we should be careful not to be too certain about what we BELIEVE to be “true”. I love your approach of challenging your own beliefs/assumptions/paradigms. This applies to body work as well as religion/philosophy, politics, and really everything.
You say that we should be more concerned about the cause, and while I agree, the truth, as I see it, is that knowing the “cause” for certain is often like knowing the “truth” for certain. There are so many relationships/connections between the psoas and other structures in the body, vertically, horizontally and in just about every direction, both direct relationships and indirect relationships through the fascia, nerves, etc. Understanding what the original “cause” is for the shortened/contracted psoas, is like the classic chicken or egg question. Sure, there are clear connection patterns to be seen, and lots of clues to be taken from posture/alignment, scars, injury history, etc. But just because you can release the psoas by finding and ‘fixing’ those other connections doesn’t mean you’ve necessarily ‘fixed’ the “cause”, especially if releasing the psoas ‘fixes’ some of those other issues, which it sometimes does.
The original “cause” is often the client’s behaviors, such as imbalanced postures and prolonged sitting in chairs, and/or injuries/surgeries. The continuation of those conditions explains why it often needs to be addresses multiple times.
What if it is because practitioners put the thought that their psoas is the problem?
Anthony,
If a therapist puts their focus on the psoas being the problem and repeating a psoas “release” that isn’t working instead of looking at the client holistically, keeping an open mind, and treating all the other issues, then Yes – That’s a problem. But that’s not what I’m talking about. I can usually achieve a relatively permanent lengthening of a previously shortened psoas within 3 sessions or less, and that’s usually with non-massage releases, and working on all the other related issues. Furthermore, I don’t typically view the psoas as the be-all-end-all cause of the clients’ problems, but rather one of several/many muscles stuck in an imbalanced holding/movement pattern. We agree that there is an unhealthy trend of undereducated people obsessing over the psoas needing to be “released” without really understanding the psoas and its relationship to other structures.
Michael
If a psoas can lengthen in 3 sessions, was that really a structural shortening?
Again, muscles are dumb and only do what the brain and nervous system tells it to do.
The psoas is just another muscle. Most problems can be sorted without thinking about specific muscles…
Hi, Can you email me, I have major abdominal pain around and under my rib and Not sure what it is from cause no one found anything, feels like tightness, bloating, I can not explain but had becoming unbearable… Morvarid.Shahbazi@gmail.com
Thanks to anyone who can help me find he right doctors in La.
Hi Pearl. I have a number of friends in the LA area – start with asking Julie Wiebe (juliewiebept.com) and go from there. Cheers
Great Post Antony! My preference is to find why its upset and correct that impairment rather than go for the “release” which is temporary, potentially dangerous as pointed out and has no real solid scientific evidence. Thanks for sharing.
Cheers – thanks Jordan. Keep it up mate…thanks also for the encouragement that there are lots of people out there trying to do the right thing 🙂
Yes! Thank you for this blog post. It is rare I actually release the psoas, although I feel confident in the anatomy. I actually prefer to release the iliacus portion along the iliac crest. But, just like you said, a tight iliopsoas is a symptom of something else. I have been treating a triathlete who was seeing a PT who (she said) aggressively release her psoas for up to 3 hours! No relief. We found her glutes together and her iliopsoas is 90% better. It’s unfortunate that some professionals are still after “the hurt”. And….my mantra…know what you know and know what you don’t know. Thanks again for a great post!
Thanks Lori. 3hrs huh? I have a 30secs rule – if it doesn’t help in 30secs, don’t bother…it is protective 🙂
“Know what you know and know what you don’t know.” – A great mantra to work by, but sometimes difficult to keep in mind. Continued success leads to confidence and confidence can become over-confidence which can lead to not being careful.
Great post Antony cheers for sharing,
I assume most people will release a psoas for one of a few reasons:
To increase ROM in hip extension, to decrease lumbar lordosis and anterior pelvic tilt or to increase hip internal rotation. If there’s any other reason I’d love people to share 🙂
In any case, I find a very non-specific pressure into the first feeling of tone/ resistance with some abdominal breathing will fix all of the above with next to no pain or ruptured organs!
I really like the technique show by erson religioso shown here: http://www.themanualtherapist.com/2011/08/technique-highlight-psoas-release.html?m=1
Harry – thanks for that. I still want to know WHY you should decrease the amount of automaic activation in a muscle before you release it.
RE3 is a nice guy but the hip extension wasn’t very specific and i will contend that he released / decreased activity of the obliques, not his psoas. Also, how does an overactive psoas result in decreased hip flexion?
Anthony,
As I’m sure you know, the psoas passes from the pelvis to the femur deep to the inguinal ligament. When you flex the hip beyond 90 degrees you are effectively wrapping the psoas around the inguinal ligament. When you do this with an inflamed psoas muscle, you put a lot of pressure on the psoas with the inguinal ligament, which often causes a sharp pinching pain at around 130 degrees or more flexion, which in turn, prevents further hip flexion.
Hmm…that’s a nice story. I doubt that is the reason why. You might want to check your anatomy and you will see that your story doesn’t hold water…that one is simple biomechanics…
Also, please call me Antony or I will call you Michal!
Harrison,
Another reason to release a shortened/contracted psoas is when there is lumbar scoliosis flexing the lumbar spine to the opposite side of the shortened psoas, since the psoas assists in opposite lateral flexion of the lumbar spine.
Hi Michael. Muscles are dumb. They only do what they are told. Better to find the reasons why it might want to do that…
You talk as if there is no return feedback from muscles to the nerves. The nervous system does tell the body what to do, but the body also tells the nervous system what to do. For example, when you force a smile or a laugh, your nervous system detects the smile or laugh and though it didn’t detect the source of amusement, it releases the hormones associated with joy and humor. It is a feedback loop, meaning that it goes both ways.
Sure. Again, how do you know it is the effect on the psoas that is generating the change you are looking for. You have to go through all the tissues in the body I talk about in this article just to get to the psoas and even then, how do you know it is the psoas that was the effect you produced?
So we can talk about feedback loops and the like but the bottom line is that the post hoc fallacy is real.
Even with the forcing a smile example, how do you know it is the release of hormones that is the released was caused by the forcing of a smile? Maybe it is because they felt stupid forcing a smile and THAT was the reason why.
I have no doubt you help people with what you do. That is not in dispute here. I just think the reasons why are debatable…I don’t cling to my reasons and I don’t think anyone else should either.
Perfect! Well weighted article. The psoas is somewhat of a hot topic at the moment, being blamed for a lot of things that it’s not responsible for. I hope this information gets out to more people – also with the message that painful massage/release techniques are usually far less effective than pressure techniques that work within pain-free ranges (intensity can be there, as long as the patient can maintain complete relaxation and full breathing cycles).
Thanks Drew. Poor Psoas does get a bad rap…
I’d also like to add you can’t really release tissues in the way that most clinicians think you can, as in mechanically. We cannot break up adhesions, scar tissue, or fascia. We can change stretch perception and muscle tone. The lighter the better. My rule is that it shouldn’t hurt at all and if so a few diaphragmatic breaths should reduce the tone and thus any accompanying discomfort.
Yep. Fair point mate. I am going to have to check the research on whether tissues change with manual therapy but i am a big believer that change is neurophysiological.
We are stuck aren’t we? We know it isn’t a “Psoas Release” but we need to use those terms because people search for them :/
email me through my site and I’ll share some research. Btw I use release too, just add ‘pain free’ to it.
If you can keep me posted on the progress of this discussion that would be great! I love to read up on the research and get a good understanding. From my understanding all change was neurophysiological as Antony mentioned. I can be contacted via email at – healthdepot@mail.com. Thanks guys!
Hi there,
I happened to read this interesting article and discussions that follows.
I must say that fascia, adhesions and scar tissues can be torn apart and rebuild.
I have developed a very unique massage technique that works on segregating fascia that glued together and even rebuilding scar tissues.
I am a massage therapist residing in Sweden. I have practised this technique on practically all my clients with amazing results.
I agree that any release in the abdomen should be performed by a skilled practitioner. The top picture is of me performing the technique (likely lifted from the website of a place I used to work), and I assure you, I was highly trained and developed excellent palpating skills before performing these techniques.
Absolutely. The picture was from google images. The post is to cause people to think about what they are doing and what else is in there
I enjoyed your blog here on psoas. One thing I like to use myself is the Yamuna balls. They are soft, especially when not inflated all the way. But as with all bodywork, all therapists should layer in gently. Even with Structural Integration, I start superficially and then go deeper. It’s also good to remember that the whole body needs to be treated because the area of pain is not necessarily the main restriction. Thanks for you sharing Anthony. Sharon Hartnett http://www.massageincolumbusohio.com
Thank you for this article. I agree. Most bodyworkers do not have enough real visceral anatomical knowledge to do deep abdominal work. There are too many important structures that could easily get damaged without this knowledge.
very much essential …
thanks sir….
keep posting….
excellent blog my friend Thank you .. I reposted it on my Facebook page… i also own a massage school in the states 24 years now and agree with you.. so thank you… By the way where did you get that one app
one app? The muscle app with pins etc? It is muscle system pro III – not entirely accurate but not too bad… 🙂
This work should be out-of-scope for most massage therapists. The word,”release” of any muscle notes a controversial meaning. I will not have this work performed on me; nor will I “practice to gain experience” on another. Thanks for the article and great photos! Possibly consider adding symptoms indicated to direct one to perform psoas work, along with peer-reviewed data indicating positive outcomes of massaging the psoas.
I’m wondering if it’s known which specific barefoot massage technique was involved, or if it was just a random use of a foot by an untrained person: you mentioned that the “coach” stepped on her psoas. This is a very important detail, as the amount of pressure possible from a persons single foot and partial body weight can be deeper than what hands/arms could dish out.
I’m a nationally certified instructor for an advanced myofascial deep tissue sports massage that uses the feet to massage. Now, our technique doesn’t work in the abdomen for exactly all the reasons you stated- its much more appropriate to use hands from a trained professional in this area. We train and certify our graduates very carefully to work with utmost safety.
However, there are other styles of barefoot bodywork out there: all broad based, deep tissue, sustained pressure from the foot. I wonder if this coach was even trained to use such a potentially dangerous tool from any recognizable source. A barefoot massage therapists feet can be used for good or evil, based on their intent, and training.
I hope all barefoot bodyworkers out there take this story very seriously and obtain proper training and certification, and stick to the protocols within that technique.
Hi.
I have seen people use feet to massage different muscles.
This woman had a health professional use fingers into the abdomen, not her feet. Sorry if there was any confusion.
Ok….. it was this line “helping people release by stepping on them (presumably to avoid any accusation of “massaging”)” and this line “Don’t just let anyone stick their fingers or foot or implement into your guts” that led me to think that some form of barefoot massage was used in this case. I’m glad it wasn’t, but I’m sorry this even happened to anyone in the 1st place.
Sorry. Those parts are my observations and warning. Karin’s story was different
I totally agree with your views in this article. I am level 5 trained sports and remedial soft tissue therapist and was taught to work on psoas but don’t because of the reasons you outline. The abdominal aorta is particularly vulnerable in my opinion. I also find that most people can strengthen or stretch this muscle without such an invasive technique. Thank you for pointing out the dangers here.
I find the timing of this article to be impeccable. I’ve been suffering with abdominal pain for over a year. I’ve had weekly massages, chiro visits, foam rolled, stretched twice a day, and nothing seemed to help. Last week I got so desperate that I ordered a DVD set I found online for releasing your psoas. I will approach this with care now. Maybe I will even return them. I need to find the cause of my discomfort and tightness. Who should I go to? My primary care doctor?
Yes Laura. Please see your doctor to clear all the possible nedical reasons first. If they are ok, find someone who can sort through a holistic view of your body to find the cause of your pain, bot just the synptoms. I hope abd pray you get some answers.
Hi, I’m a female crossfitter and had a laparoscopic appendectomy almost 8 weeks ago. Recovering from the surgery and sitting out of CF for 6 weeks was diffucult and lonely. I was cleared by my surgeon to go back to CF, and have been for 2 weeks now. I haven’t found any articles/blogs/advice etc on how to scale movements and weights to get back into WODs after abdominal surgery or what it feels like emotionally and physically . I’m guessing Karin and others may also experience similar feelings and questions…..
It is certainly a fair point Sarah.
I guess it is too dangerous for those of us that provide information because every person is a bit different.
For instance, in general, a laparoscopic appendectomy should be fairly routine but scarring does occur.
The best is obviously to go see someone who understands CrossFit, the operation you had and the effects of post surgical scarring.
Scaling – if it were me, i would go slowly and test things out slowly. It will be heavy movements that require you to hold your breath or the extension part of a kip that will be a danger.
Go slowly and gradually build up. Get confidence in the movements.
I always tell crossfitters to go to the gym even post-surgically and attend your regular class times. The reason is that crossfit is not just exercise, it is a social part of your life.
I had one patient who attended in the morning, did the warm up (scaled), did her rehab program i wrote for her and she finished in time for the cool down. For her, she would rather her arm drop off than stop training because she loves it and her “family”…so she kept going and was happy to have something useful to do while she recovered. Even sitting on the bike or walking laps of the gym is useful 🙂
Cheers
I’m UK trained osteopath and sports therapist and I do use active release techniques on Psoas as I do believe while not the primary cause of patients issues, they can be a maintaining factor as well as contributing cause of abdominal imbalance, which ultimately can lead to back and pelvic issues. One reason for this is the incorrect use of the Psoas in abdominal exercise work and the fact that we spend too long siting which I believe can cause reduction in flexibility of this muscle. I have found that in the case of over use or spasmodic tension that I can get a good level of release by addressing the muscle close to its insertion at the lesser trochanter. This is an intimate area so a full explanation of the technique to the patient is imperative as well a full communication during the process.
I agree with the above post. I am a massage therapist in the US trained in a school where I did learn all of the things you describe. I treat the muscles in the iliopsoas group fairly regularly in people who have low back pain, laterally rotated femurs, or lateral torso flexion to name just the most common instances. That being said the techniques I was taught do not entail large scale pain, are used usually near the hip crest or below that (but above the pelvic bone) where I can access the muscle with minimal interference from other muscles, and do involved a strong neurophysiological component in place of deeper pressure.
I agree that aggressive treatment through the rectus abdominus is perhaps a poor way to go about treatment and you can access the muscle without needing to push through that.
The pain relief you can get for clients who have any kind of lateral leg turn out (hockey or soccer players, people who lock their knees and laterally rotate femurs as a result, etc.) is quite remarkable and if lower spinal erectors and quadratus lumborum are contracted (anterior hip tilt) iliopsoas is almost always a player since it is forced to work in a lengthened position.
So while I think a simpler approach is better I would hesitate to scare people away from treating this muscle group. In general the core abdominal muscles are one of the areas that get work the least often but often need it.
Pingback : Barefoot Massage and the Belly… | Ashiatsu DeepFeet Bar Therapy's Blog
A good read, and useful cautions.
One correction, though, the “anterior spine” (in point 2 of the article) shouldnt relate to the actual spine. I think the author has got confused. It relates to the Anterior Superior Iliac Spine, which is the bony nobble at the front of your ‘hips’, on the ilium bone. You defo shouldnt be trying to feel your actual spine through your tummy.
Hi Matthew. The anterior spine can be felt and as I wrote in the article, care must be taken because of the abdominal aorta, inferior vena cava and associated nerves. I also mention that it is only easily felt in small, thin people.
The ASIS was not was I referring to and I wasn’t confused. The point of the blogpost was that if you are going for Psoas anteriorly, then you have to get to at least the level of the anterior vertebral body before you contact Psoas directly.
I hadn’t realised that. Thanks and sorry that i misunderstood. I find it a lot easier to find psoas by going just medial of the ASIS and asking the client to slowly raise their leg a little. This avoids the need to “find the anterior spine”.
Yep. That works too but is only one small part of the whole length of Psoas…
Hi Antony, Long time since we last spoke, I am post THR left hip one year two months.:) I regular need release of the psoas. I continue strengthening the glutes and that is helping . For many us battling hip dysplasia ,self release techniques is a daily regime . Your article is timely. I find the technique to roll to side and let gravity drop the inside contents after I have raised leg to bent position which identifies the psoas helpful. That was a technique my pt taught me. Also doing light flushing strokes with finger tips toward the belly button helpful in lymphatic clearing as well as quing a hamstring release. Here’s to healthy happy hips!
As I always ask – why do you need to daily self release?
As for a THR – you don’t have dysplasia anymore because a total hip replaces the cup and the head of the femur…so why are your muscles working to protect you?
I suspect these measures are only bandaids on the real problem.
I wish I could work that out for you but unless you come to Australia, LA, Orlando, Chicago or Pittsburgh, it is tough to help.
Thank you for this article. I just had a massage therapist stick their hand in my abdomen to test the psoas. I didn’t expect it, don’t know why it was done. It was extremely uncomfortable. I’m never letting anyone do it again. It was on the left side. It still hurts 24 hours later and I feel sick.
Iliopsoas can be effectively and comfortably released using Contract-Relax techniques followed by specific psoas stretching. Can be done prone or supine. No need to press blindly/painfully into anyone’s abdomen.
C. St. George, BCMT
Newport, Rhode Island
Fantastic post! I think well intending physios, massage therapists etc. press on structures without truly knowing what they are pressing on! Great points- couldn’t have said it better myself!
~Jessica Reale, PT, DPT, WCS
http://www.jessicarealept.com
Reblogged this on Eddie Teran, CMT and commented:
Thanks for writing this. I’ve been doing a fair amount of abdominal scar tissue work the last few months, always have to take it slow!
Favorite line, “We love to do things that ‘hurt so good!’… damaging internal organs shouldn’t be one of them!”
This article is very misleading and directed towards fear-mongering. A single incident or saying, ‘this happens more often,’ is not empirical data or statistics. Your subjective opinion is biased due to a somewhat personal experience. This is the equivalent of race baiting, by using hysteria and mis-information. I am a LMT that specializes with athletes, specifically fighters. With this premised, I will explain my disagreement to your main points.
Firstly, the deep tissues of the body often hold complex hypertension and are often neglected due to the more technical stretching and therapy they need to release them. It is a blanket statement to evoke that most issues arise from other sources of ailment, and generalizing at that. In many occupations the hip flexors suffer from chronic sitting patterns ranging from transportation to the office. As an athlete, and work on them, the hip flexors can make or break events if not fine tuned. The mobility of hip flexors and their subsequent ROM are key to full performance, in an office or in the ring.
Secondly, the therapy and body work on hip flexors vastly vary in techniques, effectiveness, ease, and ‘safety.’ Modalities including deep tissue to advanced kinetic stretching have profound effects on the hip flexors. To avoid treatment because of an isolated incident is childish. PNF stretching tools that utilize inhibitors and nerves like contract-relax and post isometric relaxation are great and easy to use, and without serious hazards. PNF techniques are also great pre and post events. In relaxed settings; slow, cautious, and well executed deep tissue techniques can be used to release trigger and tender points as well as chronic hypertonic issues. I have not once ever experienced a problem performing hip flexor releases, including athletic to heavy clients. Show us the stats that explicitly illustrate that these techniques should not be used.
Thirdly, the idea of aggressively working on a soft tissue ailment is inteslf ridiculous. What do yo mean, aggressively stabbing into the abdominal region or an aggressive plan? You are using fear mongering terminology to establish you hysteria. Here is a idea for you, you lay the client on their side and allow gravity to assist with shifting the internal tissues that are layered on top of the hip flexors out of the way. You can also flex the hip while carefully and gradually sinking deeper to the targeted muscle. I understand the inherent risk with working with layers, but you simple relax the superficial tissues prior and that’s not a problem. As far as organ and neural tissues, you can safely work around them as well, by staying lateral and close to the hip while by-passing other tissues. The pain can also come from the hypertonic tissues itself, not explicitly from surrounding nerve and organ tissues (as pain will only originate from here if the techniques are executed in a sloppy fashion or without restraint from obvious indicators like a steady pulse). YES, if you lack the sensitivity to know what you are pressing on, don’t do it.
“The sympathetic trunk”? Good god, how medial are you working?
“Most people have a Psoas that is roughly in line with the front of their spine, maybe a little bit of it anteriorly…” You don’t say.
Kidneys? If a therapist was palpating the kidneys then why do they have a license? Muscular tissue and organ tissue feel, lets just say, ‘slightly’ different.
“These courses are often restricted to physios, chiros and osteos…that is not to say your massage therapist isn’t trained, it is just much more unlikely.”
Massage Therapists come in many variations, finding one with a specialty for a specific ailment is the general idea. I am not going to go to a spa for therapeutic hip flexor releases. To generalize that massage therapists are not as qualified, hence more dangerous is misguiding and again fear mongering. Are you really stating that soft tissue professionals will be incompetent, what in comparison with physios? Specialty training and advancing your body work education obviously enhances therapist performance. To generalize all LMT is profoundly stupid.
I could say the same about CrossFit: CrossFit is a quasi real sport in that people that do CrossFit do it for CrossFit. CrossFit should therefor not use Olympic or power lifts as they do not actually enhance said fields. Repetitive and speed power lifting is an oxymoron, as such that the techniques used would also GENERALLY not pass in an Olympic program. However, to say that all CrossFit groupies have no lifting ability in an olympic or power event is profoundly stupid, as they do have gained speed, power, and strength. Therapists have the ability to safely work on the hip flexors, despite the field they are in. You cannot summarize the general abilities as you cannot assume where ailments come from without a proper client intake and interview. It is a fact that the lumbar attachments of hypertonic hip flexors directly, and mostly cause lower back pain in many clients including postural distortions.
I find this article, mis-flavored to say the least.
Pat, you make some great points, and really interesting reading. Perhaps you could edit ur post as it comes across as very aggressive and reactive rather than helpful and professional.
infact, Liz Koch speaks, after over 40 yrs of experience, to NOT get into the psoas, and yes, find out why it is out of whack. check out her site, books and such – easy info to digest and integrate on RELEASING the psoas, and move correctly to not engage it when not necessary. Also, Katy Bowman.
hi,
LMT here for over 20 yrs.
this is a great post- i abandoned aggressive methods years ago after testing out some MET techniques. it was because of a post similar to this one that i decided to change it up- there ARE better ways (if a shortened psoas is the culprit). try it out- actively engaging/firing the psoas is much more effective (and works a lot faster) at lengthening it than smooshing around in someone’s guts. no one likes their guts smooshed. pain does not equal gain.
too often we tend to take it personally when someone points out that what we may be doing may not be the best way to do things. getting defensive gets in the way of progress- methods evolve and improve. if they didn’t, lobotomies would still be a norm.
in no way do i feel this author is “talking down” massage therapists. he’s just shedding light on an issue in bodywork, proper training, and sharing ideas to improve practices across a range of professions.
Thanks Tania.
MET and similar contract and relax type therapies are nicer in general…just try to solve WHY the psoas feels it needs to be increased in activity.
In a healthy abdomen, deep work shouldn’t be a problem – I do mention that…I merely wrote this to highlight that things can get worse when a perfect storm of circumstances occur.
I think about the same things!!! I usually avoid abdominal work on clients unless absolutely necessary. There is so much going on and there are so many GI inflammatory issues. I work as slow as possible and work with the body and never too aggressive. The body is capable of healing itself as for myself a massage therapist I am only able to assist in that healing process. I believe that that abdominal region houses so much of ones emotions that if you were to even go to a trained person that has done this many times that it should be with someone you trust.
Well, it is said that 90% of your serotonin is found in your GI tract. Whether that is a significant fact or not is uncertain…
You know bones, I know muscles, attachments, nerves, viscera etc… sounds like there is a bit of animosity about massage therapists and a scare tactic going on, maybe to get more business? Im sorry you feel that way, we could be such good allys in natural health care, but we “massage therapists” are trained in releasing nearly all the muscles of the body as long as we went to a good school, also our liability insurance rate comparatively reflects the damage incurred by MTs compared to Osteos and Chiros. And don’t even get me started on Physical therapists and how they are trying to become acupuncturists on 24 hours of study when it takes a minimum of 3000 to become an acupuncturist, how much was your liability insurance annually? Less than 2% of people are harmed by massage therapy and this is typically done by men who entered the field for the wrong reasons! I would have to say that our training remains in the “non harming” area of work comparatively and is very effective. Please don’t be afraid of Massage therapists based on this blog as this is a complete fluke.
Hmm. I know bones, muscles, nerves, viscera etc etc.
There is no animosity.
I explained that it could happen to anyone including me.
The level of education for physiotherapists / chiropractors and osteopaths fairly standard as they are university degree courses. The education level for massage therapists (at least in Australia) varies in quality quite widely. So the caution to ensure your therapist (any therapist) knows their anatomy is fair.
As usual, simply choose your therapist carefully.
Hi Anthony, thank you for this, I am the author of The Vital Psoas Muscle and teach workshops all over the world, always re-iterating the psoas major needs relaxation, not pressing!
Jo Ann Staugaard-Jones
Thanks Jo Ann. If you love it, share it! Cheers
You don’t feel nauseous, you feel nauseated. Most doctors say it wrong, too, but it’s worth pointing out. Something that is nauseous makes you feel nauseated.
Very informative article, thank you. I very rarely ever try to work on the psoas, I just don’t think I need to be in there stirring the pot up, so to speak. I much prefer to introduce stretches to my client and find out what they are doing that could be contributing and things that they can do to help change it. It most instances, proper stretching and changing of certain sitting habits has done wonders.
Reblogged this on Aquarian Age Massage and commented:
This type of treatment seems to be trending right now. Here are some reasons to avoid seeking psoas release.
Pingback : Elite Chiropractic – Does Sitting Cause Your Hips To Get Tight?
Pingback : Cheap Therapy: DIY Recovery & P.T. Tools | Amanda Rego
Pingback : Cheap Therapy: DIY Recovery & P.T. Tools | Athletebiz
Hello, my friend! Your post is absolutely AMAZING! Just like you, I’m a very well trained PT, and I’ve been teaching Human Anatomy in Higher Education (Nursing and PT Colleges) for about 13 years in Brazil. Here, getting a BA in Physical Therapy is almost like going to a Medical School (at least 5 years). It’s crazy how often this kind of situation you described has been happening. I’ve seen a lot of massage therapists doing this kind of thing without having a solid knowledge related to Anatomy. Many of those professionals never dissected or even manipulated cadavers in their lives and have no clue about the risks of what they’re doing. You’re totally right. Despite a lot of professionals do try to release the psoas as a “first step” of their manual therapy protocol, it’s almost impossible to reach that muscle without irritating or damaging other structures. Also, it’s important to adress that differently from the paraspinal muscles, the psoas wasn’t designed to keep a high level of tension in order to sustain the core straight and aligned. When the psoas “takes that job”, it means something wrong is happening in the background. People that go straight for psoas release just show how they lack knowledge of basic Topographic Anatomy and also Kinesiology and Biomechanics. Those people definitely need to have Clinically Oriented Anatomy by Moore and Kapandji books as their best friends for a while to get a grip. I personally had a situation similar to this in terms of lack of knowledge happening to a patient of mine but not involving abdomen damage, fortunately. I’ve been treating a patient who has Carpal Tunnel Syndrom and a few weeks ago, he arrived complaining about edema and pain in his right knee after playing soccer with friends during the weekend. He used ice and took some AINSD but didn’t get any better. After evaluating his knee, some tests were positive to ligament tear. I referred him to a knee specialist doctor and told him to avoid any kind of physical activity or stress on the joint. Instead of doing what I told him, he talked to a friend who’s an instructor in a small gym and the guy told him I was “overstating things”. He told my patient, he had only a muscle spasm and that he should stretch it out. The outcome was a disaster: according to the NMR, my patient progressed from a partial to a complete tear of the ligament because of that. That is the kind of thing that should be a serious concern for us, responsible professionals: having unprepared people doing things that are completely wrong out there.
Hi rosane. Thanks for your kind words and scary story.
Firstly, I’d like to point out that the chiro does know what she is doing and the point was that even in trained professionals like ourselves, it can still happen. So the warning is that if it can happen to me who knows what is going on, then imagine what can happen to people who don’t know what is going on!?
Hopefully the days of trying to mechanically release something are slowly dying away.
Thanks!
Thanks for your quick reply. I didnt mean that the chiro didn’t know her job. I meant that it’s almost impossible to reach psoas due to its location. So if someone is trying to do that it does show a deficient knowledge in terms of abdominal anatomy. There’s no scientific evidence that such technique does release the muscle not to mention that some of those organs that are being compressed, squeezed are very delicate structures. So, in my point of view, it’s like putting a patient/client in risk without any guarantee of benefits. I was checking this other article about the subject and I totally agree with what’s there.
https://thesportsphysio.wordpress.com/2014/03/26/please-release-me-let-me-go/
Yes indeed. I was just making the point because the therapist my friend saw was upset that it seemed like she caused the appendix rupture. I thought ninjas made it clear enough 🙂
Yep, I got you my friend. Personally I’ve been getting good outcomes in terms of releasing, reseting and even activating muscles using dry needling associated to intramuscular electrical stimulation. It definitely helps to release the spasm and relieve the pain. 😉
I would love if any of you could recommed a practitioner in the 97470 area I could see. Love this discussion and the professional and efficacious respect along woth the practicing experience. Have a great chiro who keeps me functioning and unlocked but have dismal lumbar issues from 12 years airborne and a T3-6 recurring sublaxation (like almost daily). Really interested in massage as I know I am extremely “guarding” likely. Thanks for any help.
I’m sorry. I don’t know anyone specifically in that area. Maybe one of the others do.
I recently had this treatment at my chiropractors office and now 2 days later am having pain where I was massaged. It started out with just small pains and now seems to be getting worse. I’m icing the location with hopes of relief. I have endometriosis and hoping the pain is just irritation and nothing more serious. My next appt is on Monday a few days away and plan on mentioning it to my Dr and defiantly do not plan on having psoas release as part of my massage again. Just wondering if some pain days later is normal, maybe if you have endometriosis?
Hi Brooke – I would just get it checked by the doctor. It could be nothing. It could be something…the internet is not the place to determine that 🙁
I really hope it is just temporary pain.
Hey Anthony,
This could have been asked and answered in your comments already so I apologize, didn’t feel like reading through all 70+, but….How do you feel about getting to the psoas in the side-lying position rather than on a supine patient? I guess the thought here is that some viscera and fat will be pulled away with gravity, giving the clinician a loess obstructed path to the muscle. Safer? What are your thoughts?
It is a fair question Drew.
Ultimately, what are you trying to achieve? That’s the main question. Then we go down the rabbit hole of how does massage really work, are there such things as trigger points or are they just tender points, etc etc.
In side lying, you will still have stuff in the way.
Again, the warning is simply that there is more to getting to the psoas than looking at a muscle chart. You are most likely affecting some structure neurally anyway so find better ways.
I hope that helps.
I find this article very interesting. My husband had diverticulitis 3 years ago, with a perforated colon. He had surgery 4 months later after the infection had cleared up. Two months later, he began experiencing abdominal pain. None of his Doctors knew what to do with him, or how to help. They believed it as due to nerve damage, and began highly medicating him. We have literally seen almost every Doctor who we thought could help and have spent thousands of dollars on experiments. A few months ago, he began seeing a Holistic doctor who believes it is caused from the psoas muscle and began doing therapy on it. We were hoping for some relief for him, but have not experienced that as of yet. Thank you for posting this article, it certainly gives us a lot to think about!
Thank you Heidi. I would investigate the possibility that the pain may be neural in origin. Find someone who understands visceral manipulation perhaps?
Wow, I am now officially more confused than when I started reading this article. I appreciate the details and understand them, but where to go from here is the question, besides being doped up on tons of pain medication, effectively putting a band aid on the situation and not fixing it. I was diagnosed with pelvic tension myalgia and a tendency toward a really tight psoas by a physiotherapist trained in pelvic work. All she did for 8 months was have me do stretches and strengthening exercises like kegels. I’ve always heard that strengthening and especially Kegels are a no no for hypertonic muscles. My pain was extremely intense from top of my hip flexor through the groin and down into my left testicle on and off. I was checked by a urologist, gastroenteroligist, and after everything was ruled out, it was declared that I have CPP. I had it intensely for 1.5 years and then it went away for about 4 months. I had none of the bowel or urinary dysfunction I had with it anymore either. I did do a lot of walking during that time and no stretching when it got better. I don’t know if that is what eventually helped it or not.I had several doctors tell me it was all in my head, including my psychiatrist. I went crazy and tried to kill myself before it got better,losing my wife and son in the process. My wife always thought I was a liar and that it was all in my head too. Pelvic pain is not taken seriously enough in the world. It ruins lives and affects millions of us. It just seems like not very many people in the medical world care since it is considered a “non – life threatening condition”. I call bull $@!# on that one. It threatens people’s ways of making a living and can turn friends and families against us. Try getting disability with this or any other chronic pain condition. It is near to impossible and requires fighting that most of us debilitated by extreme pain don’t have left in us anymore. Do we stretch? Do we strengthen? Do we get our backs adjusted or have deep tissue massage? Do we have trigger point therapy or is it useless? Do we have a laparascopy to see if we have endometriosis and have it removed? I’ve heard horror stories of that creating way more problems than before they had it done. Hell,gynecologist are still recommending hysterectomies to remove pelvic pain and they cause more pain. Urologists recommend TURPs which don’t fix the problem and causes more problems too. It is a bad world we live in if you suffer with any kind of pelvic pain. No one in the medical world seems to have any real workable solutions. By the way, my pain has returned and part of my dysfunction. It is not as intense as before but has returned. To say frustration and disappointment is part of us, as sufferers, daily lives is an understatement. It is hard to trust what anyone tells us when nothing suggested works or has the potential to cause bigger problems. In addition, remember that many of us, due to work restrictions or unemployment from this evil condition, don’t have much money to be throwing at DVDs or alternative treatments costing hundreds of dollars for a maybe this will work or potentially give you more debilitating pain. Bottom line is that we need more research dollars invested in real and not possible and maybe solutions. It is a scary place we live in medically speaking when you have chronic pain. We are so desperate for answers and help that we will put our trust and hard earned dollars into a medical community that doesn’t know, seem to care to know, or work together for a workable long term solution to our problem. I’ve read books and online about chronic pain and my condition specifically and there are so many different and opposing schools of thought that where do we really turn for help? My gastroenterologist told me it was ibs for $@!#sake. Ibs? I’ve never had ibs before this condition and my ibs symptoms went away after I got better for this 4 months and hasn’t returned now that I have symptoms again. I just want you to know, as a practitioner who seems to genuinely care what we are up against with this horribly misunderstood and misdiagnosed condition. I was an athlete, writer, father, husband, and excelling worker before this hit me. Now, I’m broken financially, emotionally, and psychologically.
Hi Manwpelvicpai
1. I’m sorry that you are suffering from chronic pelvic pain. Your pain is real, I believe you. I don’t think you are making this up.
2. If walking a lot and NO stretching helped, why not try that again?
3. Believe me when I tell you that I take pelvic pain seriously. I even cohost a podcast on pelvic health…
4. I cannot help you with what to do next but there are good pelvic pain PTs around the world. Where in the world do you live? Maybe I can find a few names for you?
5. For pain management information, body in mind, NOI, PainScience.com are good places to start
6. I know you feel broken in so many ways. But you aren’t. You are here and you still together. Keep seeking!
In #MassageWorldmagazine this month is an article about Emmett Technique and the use of the psoas release technique, taught on the first day of the first training module. It uses one finger between the bottom two ribs and one finger near the tummy button to perform the release with a gentle pressure and is very effective, I can confirm.
Anthony Lo: Thank you: This blog has been amazingly informative. Though not in the healing profession, (elementary school teacher) I have an extremely sensitive psoas and I’m determined to heal so I’ve read a lot about this mysterious, huge , all important muscle over the past few years. Ever since I herniated my lumber 4_5 spine in 2010, I’ve had hip issues. I did not before. Today, I can no longer wear clothes that touch the waste. I’m curious if any one with illios-psoas issues feel lasting pain after wearing clothes with elastic that hit the waste or groin.
Maybe your problem is not with the psoas but something else and the psoas is reacting?
Great post! Thankyou for sharing such detailed information! ,I appreciate it! It helps me learn more to be a better massage therapist! 🙂
What about self-release through GENTLE stretching or VERY gentle rolling on a soft 6-inch therapy ball? My massage therapist is convinced that this would help myriad problems associated with my scolosis and consequent equinus. I have done nearly everything else to help: orthotics through a podiatrist (who diagnosed the equinus), chiropractic that has reduced my curve significantly, tons of deep tissue on my legs and back by my MT, home care through stretches and strengthening under a PT’s care.)
Thanks!
Hi Lauri
So long as you have nothing wrong with your internal organs, and it doesn’t hurt, it is unlikely to cause harm. But unless you are very skinny (like a model), it is unlikely to get into the psoas.
We have so many nerves and muscles between the psoas the the outside of the body, if “releasing the psoas” was beneficial, it is likely to be from other reasons.
Thank you for this article. I had my psoas worked on for the first time two days ago. I was okay right after, but two days later I’m still sore and my GI tract is rumbling. The massage therapist asked *me* to locate my left psoas muscle by moving my hand several inches to the left of my navel. She then began squeezing that area. Pain number 3-ish/10. I asked if there weren’t organs there that were being mashed and she said (direct quote) “I don’t know about organs, I just know about muscles.” I was stunned. Even I know it’s the spleen on the left side. Will definitely not work on this area again!
Yeah, I wouldn’t be so hasty to get that done again!
The truth is when massage therapists gradual they basically are educated in muscle and of course should know anatomy and some physiology , but it is up to each practioner to continue to educate themselves. If you do not know …look for an answer before you leap.
Pingback : psoas injury | HipFlexorz.com
Pingback : Today: Two things to stop doing. Monday: Three things to start doing. – Dynamique Health
Hi, Anthony. Just kinda ended up where I was supposed to as
I read your post. I am grateful as a massage therapist for the detail and knowledge you present.
I never go too deep and never done harm, but now grateful for the further detailed knowledge. Kudos for sharing !!!👍🏻😊
Hi. I can appreciate this article and information. However, this is an extremely rare case. I’ve been practicing NMT for 7 years. I specialize in releasing the Deep abdominal muscles including the Iliopsoas. I get excellent results with my technique but it is rather uncomfortable if the muscle is in a state of dysfunction, or in deep spasm.
I am also recovering from a disc replacement 360 fusion. Releasing the Iliopsoas has been key to my rehab, and it what still holds me back and gives me trouble to this day.
I have to stretch and work this muscle everyday on myself in order to get relief. I can’t imagine having this pain ad not having someone to release it.
Is my professional opinion that no one should be applying pressure to the abdominal cavity with a foot. This should only be done with the hands since you will be able to feel more with your fingertips. Using your foot would be a contraindication for abdominal work. How can you feel to deviate the visceral organs?
There are definitely numerous reasons to be cautious when working the abdomen and the therapist or doctor should be Highly Trained, but it is extremely important to address in order to be thorough with the therapy and give the patient relief.
Hi trisha.
Appendicitis from massage would be rare. I believe I wrote that. It still happened
Have you ever considered why the muscle is in spasm? Maybe it is on because it is trying to protect something.
Maybe after you “release” it, it comes back because you have t dealt with the real problem and instead of it holding you back, you actually need to seek out someone who can properly work out why your muscles are behaving this way – obviously I don’t believe the disc replacement is the reason why because plenty of people have had this and not needed the constant releasing of their psoas.
It is my professional opinion from working as a Physio for 20+yrs that if anyone has to do daily work to their psoas/iliopsoas, the true problem hasn’t been dealt with and the poor muscles should be left to do its job and find someone to figure out what is truly going on.
Also, stop digging into people’s tummies for all the reasons I wrote in this blogpost. Thinking you can bypass everything and get to the muscles in the first place is a massive assumption.
I respect your opinion and always proceed with caution when working the abdomen at all.
It is usually the last resort after working other muscles on the body and muscle testing for strength and weakness.
It is only addressed with moderate pressure, to be cautious of the visceral organs, while in communication with the patient.
A thorough therapist or doctor will address or stretch the psoas muscle in order to give the patient relief.
I work everything in and aground the abdomen, starting with the obliques and transverse abdominis, and working my way deeper. It isn’t always Psoas but a majority of the time it is. Especially since the psoas muscle sandwiches the lumbar spine. If there is any rotation in the spine at all it will be effected and possibly could be the missing piece of someone’s healing.
I am definitely not saying everybody should be working the Psoas. They should not. You need extensive training, which I have. However, it should not be left out as an option of therapy if you have been working with a patient and this is what they need.
As far as my particular case goes, it is very complicated. I had a grade 3 spondylolisthesis and herniated a disk in a car accident. I had the fusion 3 years ago. I work on myself daily to make it through the day but I also have 2 therapist and an Amazing Chiropractor that I work with. My situation is extremely complex. Psoas is definitely involved since it was shortened from the longevity and rotation of my injury. Adductor Magnus, TFL, IT band, and obliques also play a big role.
Again, I am not saying it should always be worked. I’m just saying it should not be left out as an option of treatment.
I will continue to address of my patient’s Psoas ( with caution). If we find that’s what they need or if they request it, which I get often bc they know the relief, I will help them.
Ok. We will have to agree to disagree.
Muscles are dumb. They only turn on and stay on if they are told to. Finding out that reason is the key 🙂 Good luck!
A few years back had a practitioner perform the deep abdominal pressure technique with his fingers after i mentioned i had a tight psoas during the consultation, even at that time the idea of poking around in those areas with such forcefull pressure was concerning to me as it seems like common sense you could be pressing on vital organs, nerves or ateries. I asked him during how safe the process was since in was in alot of pain and was told the worst would be needing to go to the toliet afterwards and somewhat naively i allowed him to proceed, i must say the pain was almost unbearable around a 9/10 far from the 2/3 suggested in this article yet regretfully i let it continue and neither my severe discomfort at the time didn’t seem to phase the practitioner at all either but regardless in the end received no benefit at all in regard to improving function or releasing the psoas and was quite sore for quite some time afterwards, could such practice if done incorrectly possibly effect the function the bladder long term, or the erge to urinate? Thanks.
Hi Dave. It is possible to develop symptoms of pelvic floor dysfunction from the physical nature of the massage but I would have thought that would be rare. More likely is that it might have developed from a reaction to the pain.
Either way, if you experience bladder symptoms, you should see someone about that.
Pain scales vary tremendously based on how they were created and what the numbers represent. (Don’t get caught up in the actual number. )
Instead work within the clients comfort level, whatever the actual number.
(In Active Myofascial Therapy we use a “RPC” scale which is rate of perceived comfort. (7-8 is the highest it should ever be and it’s subjective from the clients perspective)
We suggest it should never be more than what THE CLIENT considers a “good hurt”–even when cautious there can still be serious issues. I’ve observed it’s smart to always stay in their comfort zone.
And just for the record, we never suggest going into the abdomen to get to the psoas.
Hi Anthony,
Interesting and informative read, though it seems like you never think the psoas is a problem. I agree that most massage therapists (including myself) do not have adequate training in psoas release upon graduating. I ended up taking advanced training with a massage therpaist/chiro who works specifically in the psoas because of my own abdominal/pelvic pain. I had a uterine tumor the size of a honeydew melon grow towards my left side and wrap my uterus partially around my back. After the surgery my uterus is is slightly off center and I would intermittently experience pelvic pain. Upon taking this class, I was able to pinpoint the pain when having my psoas released. Of course I can’t say what kind of scar tissue is built up in there and what other muscles are contributing, but I do know the psoas tension comes about a week before my cycle begins and feels relief with release. There is never pain upon release, and because the work is done while I’m on my side with my knee bent,using a soft fist, there never feels like any aggressive digging is happening. I have chronic QL tightness and I know that must be a contributor as well. I believe massage should never be painful even when working deep. My psoas release feels good! Would love to hear your thoughts.
Hi Charlotte,
Thanks for your comment and story. I hope the tumor was benign and you are well.
There are a lot of beliefs woven into your story that need to be challenged – not necessarily because they are wrong but because it is hard to see other things if these beliefs form the basis of how you approach problems.
1. What does it mean to “release” the psoas? What exactly is being “released”?
2. Your uterus is slightly off centre and you experience intermittent pelvic pain – are the 2 things actually linked?
3. Again, was it your psoas that was being released – it doesn’t matter about the position…to get to the psoas, you have to go through a multitude of other tissues to before we get to the psoas
4. scar tissue – is it relevant? How can you tell?
5. What other muscles are contributing including your chronically tight QL – why are they contributing? Why are they “on” or “active”? Muscles are dumb – they only turn on when they are told to…so why are they “on”?
6. You said that “psoas tension” comes the week before your cycle begins…is it the psoas? Would a real time ultrasound show a change in the psoas size or activity?
7. Again, you describe the position for your psoas release but assume it is the psoas that is being “released” – from what we are still uncertain!
8. Your psoas release feels good – I’m happy. I support the fact you feel better when this technique is being done to you but I challenge whether it is what you think it is. We want to build stories to explain what we think is going on but really we don’t know for sure. Would you be happy to describe it as an oblique release? or a rectus abdominis release?
What if it is your superficial nerves that are upset? What if it is referred pain from elsewhere? What if there is another explanation for what you are going through?
How wedded are you to the psoas explanation?
BTW, I don’t think the psoas is often the main problem…maybe sometimes the attachment onto the leg especially in young people but not often in the spine. I think it reacts and contributes to problems but if you deal with the other issues, it settles down. I would need some serious evidence to convince me that the psoas is the primary contributing factor in a given presentation.
I hope that helps!
Anthony,
You almost seem to believe that the psoas is never the problem as if you are fanatically certain of your newfound paradigm with a religious zeal. This seems to contradict an earlier comment you made about being careful not to be too certain of what you believe to be “true”, unless I misunderstood that comment.
Anthony,
There is a lot of new research that indicates that scar tissue from surgeries is a leading cause of pelvic pain in women. It makes perfect sense. If you cut into that area, you are cutting through layers of muscle, and fascia as well as other tissues; scar tissues form where many of your incisions were and this twists and binds the fascia as well as changing the way the muscle fibers line up; now things don’t function the way they were designed to and you don’t move the way you were designed to; all of this dysfunctional movement leads to increased tension, strain, compensation, and pain. About a week before the period begins, there is an increase in blood flow and increased sensitivity in the pelvic region, so tissues swell, adding more tension to tight, bound-up fascia, which is connected to the fascia of the psoas, adding tension to the psoas, and other swollen tissues press against the psoas.
If I’m reading your collection of comments correctly, you seem to be advocating an interesting theory that the deep pain that people feel, which is quite clearly different from pain on the skin all has to do with nerves on the skin, regardless of where the perceived pain is, and that if you reprogram the nerves to stop feeling this pain, the problems within, which are merely reactions to this glitch in the superficial nerves, will all go away. Am I reading your hints properly? If it sounds like I’m oversimplifying it is because I don’t have all the details which you haven’t revealed here. If it sounds like I’m incredulous, it’s because I am, but I’m willing to entertain your theory if you can explain it better.
No. It is broader than just nerves in skin.
Perhaps tell me this…what is pain?
Seeing as one’s brain can be reprogrammed through hypnotherapy to perceive a typically “painful” stimulus as pleasurable, I would have to say that pain is the instinctive action of the brain interpreting stimulus as a threat to self-preservation. However, if you use some sort of technique to reprogram the brain not to perceive the pain in a certain area, when the pain is caused by a harmful problem, that doesn’t mean you’ve solved the problem; it only means that you’ve eliminated the symptom, in which case you may as well be prescribing opioids.
That’s one way to look at it but it is a very biomechanical way of looking at it. What if the problem is actually in the neurophysiology of the brain? The psychology of the person? The social context of the patient?
The psoas can be a problem. Just nearly always nowhere near as much of a problem as people think.
Give me a situation with a muscle where manual therapy is *needed* and results cannot be obtained any other way…
Hi Antony,
First of all I’m a physical therapist. I experience chronic low intensity back pain for 3-4 years (located at the lower low back on the left). I had Osgood Schlatter when i was 14-15 (it was hurting my quads a lot 8-9/10 pain scale).
The physical therapist i see works a lot on my left psoas, fascias and left iliocostalis. It makes my pain lower but it’s still there. (other muscles are fine and there is no articular dysfonction).
In this case, do u think working on the psoas/fascias is worth it ?
PS : if u need further information to think about my case study, ask me 🙂
Hi clement.
In this case, do I think working on the papas and fascia worth it?
First of all, there is too much to do in an examination to give advice so I won’t comment on your case.
If I had a patient who had some pain relief but nothing long lasting, I would give up on that morality and try something else.
First, thank u for the answer, indeed i think that the REAL question I wanted to ask u is : Does Osgood Schlatter condition can affect fascia of psoas and being the major cause of my back pain ? It’s more a theorical question than a case study. Furthermore when my PT work on left fascia of psoas it reproducts exactly the pain I experiment or the scientific littérature advocates the use of the patient response based model (reproduction of pain, centralisation …). In what way do u work u ? Search for hypomobility or reproduction of pain ?
Osgood and psoas. Likely to have a common nerve root supply, not fascial connection
Exact pain with left psoas palpation is likely cutaneous nerve issues
The way I work for persistent pain is to exclude anything obvious then teach pain free movement and improve strength and variety of ADLs 🙂
What’s ADL (sorry for my English 😛 ) ?
I just read the article u wrote about ur injury, it’s interesting because exactly the same questions are coming in my head when I feel pain or strain.
I realised that I didn’t give u all elements to understand, i’ll try to give u more :
-Osgood Schlatter when I was 14-15. Symptoms : pain in quads. I used to practice a lot football and when i was shooting the ball pain was worsening (extremely feel of strain in my left quad). I’m left-footed.
-Now : reccurrent back pain/strain for 3-4 years (i’m 22). It’s more a strain than a pain. My left iliocostalis is spasmmed when I experience pain and working on left psoas fascia make the pain/strain much better but after few days or a week it comes back. Side bending (frontal plane)to the right makes me experience strain on my left iliocostalis. Other muscles seem to be fine. I practice home body workout (I try to make a balanced program and I pay much attention to quality of movement) 2-3 a week and before workout I run ~30min (minimalist shoes : five fingers <3 ). After work-out (now it's almost everyday) I practice stretching of the whole body including specific and global stretchs. I think my main weakness is the transversus abdominis which is a little hypotonic IMO (I did specific work to enhance this muscle activation and i try to activate it when I do other exercises).
I don't want to bother u w/ my case so tell me if i am.
Do u know some structure I could have missed ? If u want to know more I can do a few tests and tell u the result of the test.
ADL = activities of daily living
Thanks for the extra information. Doesn’t change my mind
How can you have a truly strained muscle? I know it feels strained but it just feels that way (probably).
Ok, thanks !
Are u saying that : maybe the strain I feel isn’t due to muscle(s) but to another neurologic mecanism ? Can u give me an exemple to get a better understanding of ur thought ?
Hi clement.
Nerves communicate sensation. You are a Physio. I think you understand this.
Therefore irritating a nerve can make it feel like a strain.
No fascial connection between the patellar tendon and psoas? I have to disagree. Let’s see: There’s a facial connection between the patellar tendon and the quadriceps, followed by a fascial connection between the quadriceps and the illiacus, followed by a fascial connection between the illiacus and the psoas.
Of course, that doesn’t mean the psoas is the problem or that it needs to be released. Unless the OS condition was only on one leg, which begs the question, “what other musculoskeletal imbalances are still present which might have caused the OS condition on one leg and not the other?”
Michael. Fascia is everywhere. You can make a link from anywhere to anywhere.
If you read my comment and the comment I was answering, he was asking if OS can be the cause of his back pain via a fascial connection to his psoas. I replied (quite correctly mind you) that it is much more likely that a shared nerve supply might be a link, not the fascial connection.
Have a read of some of these concepts…
Lederman, E 2010 The fall of the postural structural biomechanical model – http://www.cpdo.net/Lederman_The_fall_of_the_postural-structural-biomechanical_model.pdf
Lederman, E 2010 The Myth of Core Stability – http://www.cpdo.net/Lederman_The_myth_of_core_stability.pdf and https://www.liberatedbody.com/podcast/eyal-lederman-myth-core-stability-lbp-033/
Post Hoc Fallacy
Confirmation Bias
These will be good for you…
Antony,
Thank you for supplying these links. Hopefully, these will help me begin to understand the heretofore unexplained belief system behind your statements.
Sorry about getting your name wrong. That’s another example of the brain misinterpreting stimuli. It sometimes ignores what it’s actually seeing, because of what it assumes it’s seeing.
Back sometime a go about 10 years, I did had ulcerative colitis which ended up having 2 surgeries, large bowel removal/stoma bag and j-pouch creation. Now I’ve started going gym actively and doing all the crazy abs exercises from what I felt my lower back until one day there was a click! Herniated disk! My doctor told me that I had removed large bowel that used to support against lower back spine. Wish I would know that earlier, now just light exercising and stretching..
Hmm. Maybe it was unrelated?
Your doctor’s explanation doesn’t seem logical. The bowels are not firm enough to support your spine. Your muscles support your spine. It is much more likely that your abdominal exercises were a too “crazy” and not ergonomically correct, and/or that while you were strengthening your abdominal muscles you weren’t doing enough to strengthen your back and other core muscles.
Pingback : Barefoot Massage and the Belly… | Heeling Sole
Hi Anthony….. have you ever heard of the technique which illicits and regulates the body’s natural therapeutic tremoring response – AKA TRE – Tension Release Exercises ? If not, I will let you and your readers Google it ( I am in Los Angeles) but I wanted to make sure you have TRE integrated into the conversation as one of the more gentle, hands-off techniques. It basically works by down regulating the nervous system. Feel free to find me to ask me more.
BTW. So glad to find this site. Physio-geek heaven, YAY.
Hi Mary. I just finished teaching with Robin Kerr who is being accredited in TRE. I’ve had a go at it. It didn’t do much for me but others like it. Whatever works for you. It’s a helluva lot safer than sticking fingers into your abdomen!
I am glad to hear the word is getting out about TRE. We understand the power of belief in healing so I agree.. not everything is for everyone. Thanks for your quick reply… and if you speak with Robin again soon… ask her to give me shout. I would love to meet her. Cheers
Robin Kerr. Integrated Pelvic Physiotherapy. Noosa Queensland Australia. Shoot her an email.
Thank you, sir. I will. I also work in tandem with a PT specializing in pelvic floor issues. I look forward to comparing professional notes.
Awesomesauce! Cheers
I’m curious to know what the most common “real” underlying issues to psoas can often be, since the article mentioned the psoas becoming tight is usually due to another problem and rarely a problem with the psoas itself, are there some resources I could look into to maybe explore these possibilities? I’ve been foam rolling basically all my legs, hips, and glutes, and I’ve been poking gently in where the psoas connects to the hip, and would prefer to avoid digging in the belly. My acupuncturist does needle points for the psoas which helps, but it’s never long lasting. My hip pain has been less consistently constant than the past, but occasionally flares up despite not changing much in my routines, I’m thinking it might be a combination of glute and back trigger points?
Hi Rebecca.
Apologies for the delay in replying.
The psoas is a muscle like any others.
Muscles are dumb. They just do what they are told.
Therefore, if the brain thinks it needs the psoas to be active, it will get the psoas to work hard.
Possible regions why the psoas may be overactive include any joints in the trunk and lower limbs. Given that the muscle itself attached over a long area and interfaces with many structures, the reasons are many and varied. It is also the reason why I don’t speak specifically about these as I could base a whole website on the reasons why psoas is overactive.
You’d best spend your time finding someone to help you move as many ways as possible.
Thanks for the reply! I do have pelvic tilt/rotation/Si joint misalignment, and seeing the chiropractor helps a lot, so I think the psoas problem is a trickle down effect from Si joint issues, as I get pain there, my lower back and in my glutes and lower TFL band on the opposite side of the psoas pain. I’ll probably continue with a mash of treatments along with SI aligning excersises and strengthening/activating glutes, abs, obliques, and foam rolling head to toe. Fingers crossed this does it!
Well, if you want a different take on things, let me know.
There are plenty of beliefs in your words which I think can be challenged by the science but only if you want to hear them.
Excellent article. This clearly shows that you should always consult your doctor or at the very least get advice from a trained therapist. Some thought should always be used when participating in any physical activity.
I tore my psoas and illio many years ago and went through pt. over the years, acupuncture, TRE, chiro, nfdt, have all helped. All psoas manipulation has gone through my back or stomach with fair results but no solution. After 20 years of this, I cracked the code ( for me at least). I had strained it and going through usual rehab- acupuncture and nfdt. one night the pain had awaken me and as I was laying on my side( pain side down and that is KEY) I pressed the psoas about 4 inches below my belly button) and got a fast small pain and great release with very minimal pressure. Then, I pressed same area on the pain side, and got a hit the psoas and then around 8 pops in my spine in the tailbone area. Never experienced that release and after eight months, I have zero pain since that. Would like thoughts and as well, if this helps one person by sharing, it was worth it.
I was seriously considering having my massage therapist who has been trained in the release of the psoas, to do the release procedure. This article has changed my mind. At least until I can do more detailed research on it. Thanks for sharing ,karins story.
Thanks Amy.
I would ask your therapist to maybe massage from the low ribs near the spine to the edge of your rectus abdominis (6 pack muscles) gently!!! Also check out a book on kindle which is only about USD$8 called dermoneuromodulating by diane Jacobs. It’s got tons of good stuff. Have your massage therapist read it as well!
Hi! Thanks for this article. Even though it’s quite scary to read about, I’m grateful for you for posting regarding the risks of psoas release.
Quick question. I’m in middle of physical therapy for a hip injury(with a trained US therapist) and she had done a psoas release to me twice. Both times killed me (so much pain both during the release and for a week after) and there’s no way I’m ever letting her do it again after reading about the risks here. I’m just wondering if there’s any chance that in doing the release she might have damaged something inteneral (such as one of my ovaries?). I’m a pretty thin female so I believe she was able to reach my psoas but I’m just really nervous that she also could have inadvertently caused damage to another organ at the same time (esp because she did this twice and it literally was like a 9.5/10 in pain). How likely do you think it would be? Is there anyway to confirm that there are no internal injuries? I’m honestly most concerned about my ovary because she pretty much did most of the release right where my ovary should be located (to the upper left of my uterus, above my pelvic area).
I would really appreciate hearing your thoughts. Thanks!
Hi AB – I’m sorry i didn’t find this message earlier
Therapy should never really hurt. I would let her know. The best way to assess injury is to ask a MD to help you find out.
9.5/10 pain is not really what we aim for in physical therapy!
Cheers
So glad I read this.
Very happy to have this information so early in my career. Thank you!
So then what should one do, if one has a psoas that needs to be released?
Wel, firstly it is unlikely you need your psoas“ released”. What are you releasing anyway?
Any manual therapy is interacting with the neural system via the skin so start with finding out why you have pain.
Understanding why you have pain and how to improve it is key.
For that, you need someone with skills such as mine, someone who stays up to date with the current research and presents scientifically plausible reasons why you have pain.
What city do you live in?
Hi – 3 years ago I was on my bike and hit sideways by a car, no broken bones but my back/hips were a mess. After a year of chiro & physio treatments I was feeling pretty ok but there was a lingering soreness/pain. I’ve since been diagnosed with a “contracted psoas muscle” by a chiro, 2 physio, a family doctor and a physiatrists and have been told there is nothing anyone could do for me. The best thing would be to try and strengthen my lower back muscles so they will get less sore. I’ve been diligently working on core strengthening, lower back muscles and psoas stretches but nothing seems to help. My lower back gets super tight and I feel this “dull, throbbing pain” inside my abdomen on the one side. What would be your treatment recommendations for a “locked psoas muscle”, considering the cause of it was the hit /impact during an accident? Thanks a lot for your input. It seems difficult to find professional help for this.
Hi Barbara.
I’m sorry to hear you are still suffering.
Basically I would try to alter how your body perceived information from that region with exercise and a version of manual therapy called dermo neuro modulating.
Which city do you live in?
There are many different ways to release a contracted psoas, only one of which includes manual massage. However, if stretching it doesn’t seem to help at all, I wonder if you haven’t been misdiagnosed and maybe the problem is that the painful psoas muscle is being pulled into a stretch already by other musculoskeletal misalignments, so it is counter-contracting. Often the muscle that feels pain is not the cause of the problem, but merely a symptom. When you lie on your back, does your leg flatten out for the most part, or does it lift slightly from the hip and bend slightly at the knee on the side of the painful psoas? If the leg is flat, I don’t think it could possibly be that your psoas is dramatically contracted or shortened.
I had abdominal surgery three years ago for appendix cancer that ruptured and had spread to other organs and had a total hysterectomy, appendectomy and omentectomy. Since then I have experienced a deep aching in my right groin area. Nothing has been found. Many tests later, I went to a physiotherapist (in Canada) for a severe pain radiating from approximately the same area down my thigh and around my knee. He had been doing a bit of deep tissue massage until the day that my blood pressure went sky high, I felt nauseated etc. He has since gone much easier on the treatment. No deep tissue work. The deep pain I had experienced is gone, but the aching feeling persists. Do you think I should not try to get to the bottom of this deep ache or should I see someone else? Is this a possible psoas problem?
Hi Sheila
I advocate for a gentle approach to such problems – it shouldn’t cause pain or feelings of nausea or high blood pressure!
There are many nerves in and around the area. I would be working to desensitise those.
Where in the world do you live?
My physic is now giving me stretching exercises, doing ultrasound, tens. No more deep tissue work. The original throbbing/aching I have felt now for 3 years continues. the sharp pain referring down my leg to my knee has cleared, but I remain with a tugging tightness in my groin. I’d like to find a reason for the aching in my right groin area. Do you think it might be from my surgery? I get regular CT scans and nothing is showing on them. I live in Ontario, Canada. Thanks for your reply.
Hi Sheila
Greg Lehman is in Toronto. He might have good contacts for you.
Diane Jacobs is also Canadian and she might know people who can help.
They both understand the science of pain and how nerves work and would be good to link with you.
There are many reasons why you can experience pain. It’s hard to tell without a proper assessment so the above physios would be good to sort something out with so you can get some answers going forwards.
Cheers!
My Chiro worked on my psoas at least 5-6x last year (“to release adhesions causing lower back pain”). He had me lie on my side and slowly worked in my lower ab area. By the end of the year, I was (still am) having blood in my stool (and, alas, the back issues continue!). I am now seeing a gastroenterologist to figure out the cause. I never connected the two things (psoas work and blood in stool) but this article makes me wonder whether he damaged something. Or perhaps just a coincidence? Maybe I should mention to my gastro? Thank you.
Hi.
Definitely tell your specialist and doctor about it.
I’m not saying the Chiro did any damage, just so the doctors can check it all.
Went to Physical therapy for low back pain. Think she did the psoas massage. She said, it would feel like she is ripping out my ovaries. It was painful in the moment but ok afterwards. The following day my pelvis hurts so bad. Feels like cramps. Hurts to sit and stand. Still hurts 2 days later. I hope she didn’t mess anything up. Is it supposed to feel sore?
No. It shouldn’t hurt like that. It is unlikely she did any damage but that kind of treatment is, in my opinion, unnecessary.
I am not blaming or judging your PT – I used to do things like this because I was taught to just like she probably was but I have come to realise it is not necessary.
Do you feel brave enough to let her know about this article?
Poor girl. It should never feel like someone is “ripping out your ovaries”. There is good pain and bad pain. Dull pain is okay and unlikely to cause damage except bruising if the point is held too long. Dull pain caused by pressure on a muscle should subside as the muscle softens with a few deep, full breaths and a focussed intention of relaxing the muscle. Sometimes dull pain can be intense but still dull. Sharp pain feels like tearing, stabbing, or an electrical shock and that’s the kind of pain that is more likely to cause injury, especially if sustained for more than a second.
Anthony,
This is an excellent article that has forced me to rethink manually manipulating the psoas. As manual manipulation is typically very uncomfortable for the client and I have 5 other techniques for releasing the psoas, it is usually the last approach I use, but now that you have caused me to re-examine more of the possible dangers of manual manipulation of the psoas, I will make sure that it is my technique of last resort and I will teach my Taoist Deep Tissue students likewise. If you don’t mind I will reference your article. I do still believe that the psoas can be safely and effectively massaged but you clearly need to be incredibly careful and absolutely certain that what you are touching is indeed the psoas.
Thank you. You have to also be mindful that you cannot tough anything in isolation…
Antony,
Do you have any good referrals for physios in Chicago?
Hey Jake – Look up Sandy Hilton and Sarah Haag at Entropy Physio. They can either help you or direct you to someone closer. I’m sure there are lots of physios that are good…just got to find them!
Cheers
Hi Antony, I am in the Philadelphia/Southern NJ area. Do you have a referral in my area? I also travel to Orlando on business from time to time.
Thanks!
Hello, I just read your post and wonder if you can give me some advice. I am seeing a Physical therapist and on the day she discharged me this past Wednesday, she did a Muscle energy thrust to my iliac area stating i had a longer leg. now I am in a lot of pain and can feel the joint area near my trocantor and it feels very weird stiff and aching. she said she didnt do anything major but would this pain be normal? Im not sure what to do and read about bursitis and wonder if that was affected due to the motions. previously in my therapy i only did stretches and nothing like this so i am very concerned. thank you for any feedback. i dont know if i should go back to her or see another dr.
Antony, do you have any good physio referrals in Denver, Colorado? I have so many issues I don’t even know where to start. All issues resulting from a bicycle crash and resulting fractured hip over a year ago. My entire pelvis is a mess. Muscle atrophy and weakness from prolonged limited movement, all sorts of overcompensation issues from favoring the good side over the injured side, etc etc.
Hey Marco – I’m sorry, I don’t have any specific contacts off the top of my head in Colorado. I can put the word out and see though!
Thank you, Antony. I appreciate it! Cheers.
Ok.
I don’t know these people but this is what my Facebook fam told me.
Zach Harmon
Emily Kelly
Dawn Mac Conkey-Sandalcidi
Stacy Wilson Soappman
Michael Polon
Nicholas Studholme
Again, I don’t know them so interview them.
You need a biopsychosocial approach.
Oh man, so glad I checked back here. Thanks a lot Antony. I’m going to do some research on these folks. I really appreciate you taking the time to get input from your Facebook fam.
Cheers!
No problem Marco – let me know how you go
What primary and secondary issues could cause tightness and painful knots in the psoas? I was sent to pelvic floor physical therapy for a stabbing pain in my lower right side. The physical therapist found the site of the pain. She said my psoas was like a tight rubberband with a large knot. She did a lot of very painful manipulation to the psoas muscle, and she also did dry needling to the muscle which lead to bruising and a stinging pain. The pain has not resolved, and I am curious at to what may be causing it.
Hi Melanie
Lots of things can cause tenderness.
Muscles are dumb – they just do what they are told.
Something else is causing your psoas (if that is really what it is) to try and protect you.
The main groups of things I think of are the following 6 headings
1. Joints
2. Muscles
3. Nerves
4. Internal organs and medical conditions
5. Psychological and Sociological contributing factors
6. Strategies for performance and function – how you do whatever it is you are doing.
A good therapist should be trying to prove themselves wrong, all the time, not try to prove themselves right.
PLEASE HELP. I used a tennis ball on myself to massage this area. I didn’t learn or hear about doing this anywhere.. it was just something I thought to do. It left my outer thigh numb, so I thought I did something to my femoral nerve. Couldn’t fit into MRI.. and I surpass the weight limits for an open MRI. Now my inner thigh is tingling & going numb. What do I do? What kind of specialist should I see?
Hi kelley
It’s hard to say what you should do.
Start with your local doctor.
You’ll probably get referred to a neurologist.
If everything is clear, then try to find someone who can help you through pain.
So if your chiropractor said the cause of your pain is indeed a tight psoas muscle and suggests massage what should I do.
Hi Jody.
You have 2 choices:
1. Accept what they say and let them do it.
2. Get a second opinion.
I can’t tell from here if the Psoas is the source of your trouble but my default is that it isn’t…option 2 is my biased opinion 🙂
Pingback : Articles Of The Week March 11, 2018 – The Massage Therapist Development Centre
Pingback : Hip Flexor Pain: Causes, Treatments, and Evidence - Massage And Fitness Magazine
I have an ataxic condition, and my mom finally talked me into seeing a TCM clinician. During the session, I was aggressively needled across my entire ab wall and anterior hip.
I’ve really tried not to get worried but it’s been almost 2 weeks now and the stretch reflex in my hip flexors are still not 100% back. My ataxia and gait has worsened. I don’t have that reflexive contraction that occurs during hip extension/terminal stance and my stride length has shortened drastically and my hip/knee buckles. Also developed new back pain as the entire area feels very loose and uncontrolled.
Do you know if the stretch reflex will eventually come back and how long will it take? Or have I been sent down a slippery slope? I am already pretty hypermobile and physically deconditioned. Is there something I can do to speed this up? I hope this doesn’t sound like actual nerve damage or something.
I talked to the clinician over the phone but she kept pedaling the same ‘feel to worse to feel better” narrative.
Sorry for the reply on this very old post….no one to talk to about this
Hi Gabriel. It is difficult to give a proper diagnosis and advice. It’s actually unethical and healthcare professionals shouldn’t be doing so.
I’d suggest going to the doctor and explain what has happened. Do you have a neurologist?
It could just be coincidence.
Best to check it out with a specialist doctor first – not that I think you have something bad or anything, just to rule that stuff out first.
Let the practitioner know again what has happened and how it hasn’t gotten better yet.
Your words have a way of comforting and uplifting those who read them.
Thank you
Hi Antony! Do you by chance have any physio referrals in New York City? I have been having right abdominal pain for about 2 years now and have had every procedure under the sun done to try and figure out what it is. The pain radiates to my lower back, glue muscle, and sometimes down the front of my thigh. No doctor can figure it out. I am seeing a Chiro and he thinks its psoas related and does a light psoas release which causes me to have more pain for about a day, but then once that subsides, I do feel a lot better! Curious to get other opinions on this though, so any advice you have would be super helpful! Thank you.
Hi. Is there a particular borough you are in? Also can ask your providers about superior cluneal nerve irritation. Let me know!
I am in the East Village, but any borough works. Thank you!